The best treatment for Crohn’s disease is a topic that many patients struggle with, as finding the right approach can be challenging. However, with the help of expert insights, individuals can navigate their options more effectively.
From medication management to dietary changes and lifestyle modifications, various strategies can be explored to help manage the symptoms of Crohn’s disease. Patients need to work closely with their healthcare providers to find the best treatment plan that suits their individual needs and preferences.
By staying informed and proactive, individuals can take control of their health and improve their quality of life despite living with Crohn’s disease.
As a chronic inflammatory disorder of the gastrointestinal tract, Crohn’s disease affects many people globally. It is characterized by inflammation of the digestive tract, which can cause a range of symptoms, including abdominal pain, severe diarrhea, and weight loss.
While there is no cure for Crohn’s disease, there are several treatment options available, including common over-the-counter painkillers like ibuprofen, naproxen sodium, diclofenac sodium, and others, to help manage symptoms and improve quality of life.
In this blog, we explore Crohn’s disease treatment options like medication, surgery, and emerging therapies. We also cover lifestyle adjustments and home remedies.
Whether you’re newly diagnosed or a long-time sufferer, this blog offers insights for informed decisions on intestinal tract treatment, recommending a combined approach of surgery and medication for reduced recurrence risk.
Key Highlights
- Crohn’s disease is a chronic inflammatory bowel disease that affects the digestive tract, causing symptoms such as abdominal pain, severe diarrhea, and weight loss.
- Treatment options for Crohn’s disease include medication management, surgical interventions, and emerging therapies.
- Medications commonly used to manage Crohn’s disease include anti-inflammatory drugs, immune system suppressors, and biologics. Medications like these may relieve inflammation and help with symptom management.
- In some cases, surgical interventions may be necessary to remove damaged tissue or address complications such as strictures or fistulas.
- Emerging therapies, such as stem cell therapy and small molecules, are being studied as potential treatment options for Crohn’s disease.
- Lifestyle adjustments and home remedies can also play a role in managing Crohn’s disease, including dietary considerations and stress management techniques.
Understanding Crohn’s Disease
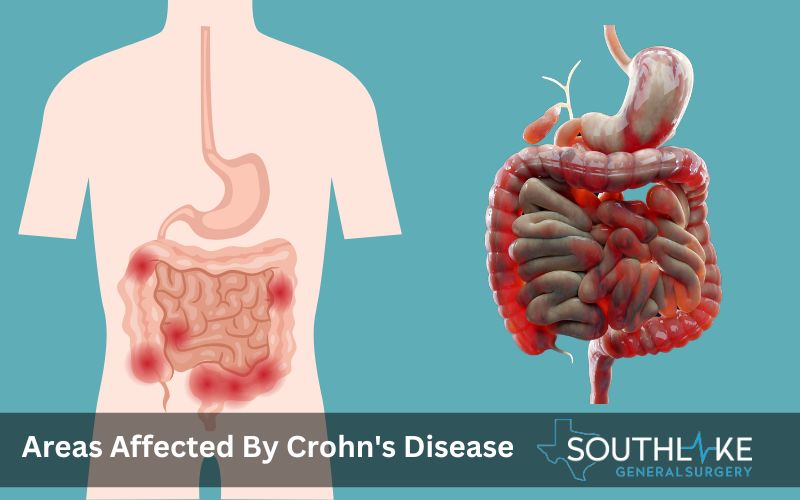
Crohn’s disease is a type of inflammatory bowel disease (IBD) that takes place in the gastrointestinal (GI) tract and is characterized by repeated inflammation. It can affect any part of the digestive tract, from the mouth to the anus, but most commonly affects the small intestine and the beginning of the large intestine.
The exact cause of Crohn’s disease is unknown, but it is believed to involve an abnormal immune response in which the immune system mistakenly attacks the cells in the gastrointestinal tract.
This chronic inflammation, characterized by clusters of inflammatory cells known as granulomas, can lead to a range of symptoms and complications.
What is Crohn’s Disease?
When it comes to the gastrointestinal system, Crohn’s disease is a chronic inflammatory condition that has a unique influence. Both ulcerative colitis and Crohn’s disease are instances of inflammatory bowel disease (IBD), although Crohn’s disease is one of the most common types of IBD diagnosed in people today.
Ulcerative colitis primarily affects the colon and rectum, whereas Crohn’s disease can affect any region of the digestive tract, extending from the mouth to the anus. Furthermore, a greater chance of developing colorectal cancer is associated with Crohn’s disease.
In Crohn’s disease, the immune system mistakenly attacks the cells in the digestive tract, leading to chronic inflammation. The following symptoms may manifest as a result of this inflammation:
- abdominal pain
- severe diarrhea
- fatigue
- weight loss
The small intestine and the first portion of the large intestine are common sites where symptoms manifest themselves in individuals who have been diagnosed with Crohn’s disease. However, the inflammation can occur in patches and can involve any part of the digestive tract.
The inflammation can also extend into deeper layers of the bowel, leading to complications such as strictures, fistulas, and abscesses.
Antibiotics, such as ciprofloxacin and metronidazole, are frequently prescribed to reduce inflammation and promote healing in people with Crohn’s disease. Pain relievers can also be used to help manage the abdominal pain associated with the disease.
Causes and Risk Factors
The exact cause of Crohn’s disease is not fully understood, but several factors are believed to contribute to its development. One of the main risk factors for Crohn’s disease is a genetic predisposition, as it tends to run in families.
However, the presence of a family member with Crohn’s disease does not entail a definite probability that an individual will develop the condition.
Moreover, research has indicated a rising prevalence of Crohn’s disease among individuals of Black ethnicity residing in North America and the United Kingdom, implying that ethnicity may contribute to the onset of the condition.
While there is no firm evidence that any foods cause Crohn’s disease, certain things seem to aggravate flare-ups, making it important to maintain a healthy diet and track personal triggers through a food diary.
Other factors that may increase the risk of developing Crohn’s disease include abnormalities in the immune system, environmental factors such as smoking, and certain medications such as non-steroidal anti-inflammatory drugs (NSAIDs).
Additionally, it is more prevalent among specific ethnic groups, particularly persons of Ashkenazi Jewish ancestry who are at a greater risk.
It is important to note that while these factors may increase the risk, they do not guarantee the development of Crohn’s disease. The exact cause of the condition is still not fully understood, and further research is needed to better understand its origins.
Symptoms of Crohn’s Disease
Symptoms of Crohn’s disease can vary from person to person and depend on the severity and location of inflammation in the digestive tract. The most common symptoms include:
- Abdominal pain: This is one of the most common symptoms of Crohn’s disease and is often experienced as cramping or sharp pain in the abdomen.
- Severe diarrhea: Chronic diarrhea, often accompanied by loose stools, is another common symptom of Crohn’s disease.
- Weight loss: It is possible to lose weight without trying due to the chronic inflammation and malabsorption that come with Crohn’s disease.
- Fatigue: Many individuals with Crohn’s disease experience fatigue, which may be due to the body’s immune response and nutrient deficiencies.
- Other symptoms: Inflammation can impact different areas of the body, including the skin, joints, and eyes; persons with Crohn’s disease may also encounter less appetite, mouth sores, blood in the stool, and a host of other symptoms.
It is important to seek medical advice if you are experiencing any of these symptoms or if you are concerned about potential complications, such as colon cancer, that may arise from Crohn’s disease.
Additionally, if you notice any signs of infection, such as fever or increased pain, it is important to seek immediate medical attention.
When to Seek Medical Advice
If you are experiencing symptoms of Crohn’s disease, it is important to seek medical advice for a proper evaluation and diagnosis. Timely identification and intervention can effectively control the condition and mitigate potential complications.
It is recommended to consult a healthcare professional, specifically a gastroenterologist who specializes in digestive diseases if you are experiencing persistent abdominal pain, severe diarrhea, unexplained weight loss, or other symptoms associated with Crohn’s disease.
In addition, seeking medical advice is a good idea for obtaining accurate and reliable health information about Crohn’s disease.
Healthcare professionals can guide symptom management, treatment options, and lifestyle adjustments that can improve quality of life and overall well-being. They can also address any concerns or questions individuals may have about their condition, including the use of a feeding tube for enteral nutrition.
It is essential to have open and honest communication with healthcare providers to ensure the best possible care and support for individuals with Crohn’s disease.
Diagnosing Crohn’s Disease
For a definitive diagnosis of Crohn’s disease, a doctor will look over your medical records, do a comprehensive physical, and do diagnostic testing. The diagnostic process aims to rule out other conditions with similar symptoms and to identify specific signs of Crohn’s disease.
Medical history evaluation: Healthcare professionals will review the patient’s medical history, focusing on the symptoms and family history of Crohn’s disease or other inflammatory bowel diseases.
Physical examination: A physical examination may be performed to assess for signs of Crohn’s disease, such as abdominal tenderness or swelling.
Diagnostic tests: Several diagnostic tests are typically employed to confirm the diagnosis of Crohn’s disease. These tests include:
- Colonoscopy: This procedure involves inserting a flexible tube with a camera into the colon to visualize the interior lining and collect tissue samples for biopsy.
- Imaging tests: Imaging tests, such as CT scans or MRI scans, may be used to visualize the digestive tract and identify areas of inflammation.
- Blood tests: Blood tests can be done to check for signs of inflammation, such as elevated levels of C-reactive protein or white blood cells.
- Capsule endoscopy: This procedure involves swallowing a small, pill-sized camera that takes pictures as it passes through the digestive tract. It provides detailed images of the small intestine, which is often difficult to visualize with other diagnostic tests.
These diagnostic tests, along with the patient’s symptoms and medical history, help healthcare professionals make an accurate diagnosis of Crohn’s disease.
Preparing for Your Doctor’s Appointment
Preparing for your doctor’s appointment is essential to ensure a productive and informative visit. To help you prepare ready, here are a few tips:
- Make a list of symptoms: Before your appointment, write down all the symptoms you have been experiencing. Include details such as when the symptoms started, their frequency and severity, and any factors that seem to worsen or alleviate the symptoms.
- Gather your medical history: Collect any relevant medical records or test results related to your symptoms or previous gastrointestinal issues. This information can offer valuable insight for your healthcare provider.
- Prepare a list of questions: Write down any questions or concerns you have about your symptoms, diagnosis, or treatment options. In this way, you can be confident that the appointment will cover all your concerns.
- Be ready to discuss lifestyle factors: Your doctor may ask about your diet, exercise routine, stress levels, and any medications or supplements you are currently taking. Be prepared to provide detailed information on these topics.
By preparing for your doctor’s appointment, you can ensure that you make the most of your time with your healthcare provider and get the answers and guidance you need to manage your Crohn’s disease effectively.
Treatment Options
Treatment options for Crohn’s disease can vary depending on the severity and location of inflammation, as well as individual patient factors. The objective of treatment is to alleviate inflammation, control symptoms, and enhance overall well-being. The main treatment options include:
- medication management
- surgical interventions
- emerging therapies.
The choice of treatment options depends on factors such as the severity of symptoms, disease location, and individual patient preferences.
Healthcare professionals work closely with patients to develop personalized treatment plans that optimize symptom management and long-term disease control.
Medication Management
Medication management is a crucial aspect of treating Crohn’s disease. Several types of medications may be prescribed to reduce inflammation, manage symptoms, and promote long-term disease control.
- Corticosteroids and aminosalicylates are two examples of anti-inflammatory medications that may reduce gastrointestinal inflammation. These medications can provide short-term relief but are generally not used for long-term management due to potential side effects.
- Immune system suppressors, including azathioprine and methotrexate, work by suppressing the immune response that causes inflammation. Although these treatments can help with symptom control and flare-up frequency reduction, they do come with the risk of infections.
- Biologics are a relatively new kind of medicine that targets particular proteins that are part of the immune response. They can help reduce inflammation and manage symptoms, especially in individuals who do not respond well to other medications. One potential downside of biologics is an increased risk of infection.
It is important to work closely with healthcare professionals to monitor the effectiveness of medications, manage side effects, and adjust treatment plans as needed.
Medication management is most effective when it is accompanied by frequent follow-up appointments and open communication.
Surgical Interventions
Surgical interventions may be necessary for individuals with Crohn’s disease who experience complications such as strictures, fistulas, or intestinal obstructions. Surgery aims to remove damaged tissue, relieve symptoms, and improve overall digestive function.
Common surgical procedures for Crohn’s disease include:
- Strictureplasty: This procedure aims to expand a constricted portion of the intestine to enhance the movement of digestive contents.
- Resection: In cases where damaged sections of the small intestine or large intestine cannot be repaired, a resection may be performed to remove the affected portion.
- Fistula repair: Surgery can be used to close fistulas, abnormal connections between different body parts caused by inflammation.
- Colectomy: In severe cases, removal of the entire colon may be necessary to alleviate symptoms and improve quality of life.
Those suffering from Crohn’s disease may find some relief through surgery, but it does not cure the condition.
It is important to discuss the potential risks, benefits, and long-term implications of surgery with a healthcare professional to make an informed decision about the best course of treatment.
Emerging Therapies
The therapy choices for Crohn’s disease are being enhanced through the exploration of emerging therapeutics. These therapies offer potential advancements in managing symptoms and achieving long-term remission. Some of the emerging therapies currently being studied include:
- Stem cell therapy: The immune system and injured tissues can both be repaired by stem cells. To speed healing and lessen inflammation, stem cell therapy is being studied as a potential treatment for Crohn’s disease.
- Small molecules: Small molecules are being developed to target specific molecular pathways involved in the immune response and inflammation seen in Crohn’s disease. These molecules aim to provide more targeted and effective treatment options.
- Clinical trials: Ongoing clinical trials are testing new medications and treatment approaches for Crohn’s disease. These trials help evaluate the safety and efficacy of emerging therapies and provide opportunities for individuals to access innovative treatments.
It is important to note that emerging therapies are still under investigation and may not be widely available.
However, they hold promise for the future of Crohn’s disease treatment and may offer additional options for individuals who do not respond to conventional treatments.
Lifestyle Adjustments and Home Remedies

In addition to medical treatments, lifestyle adjustments, and home remedies can play a significant role in managing Crohn’s disease and improving quality of life. Some recommended lifestyle adjustments include:
- Stress management: It is important to note that stress has the potential to worsen symptoms of Crohn’s disease. Stress management techniques include regular exercise, meditation, and relaxation exercises.
- Special diet: While there is no specific diet that works for everyone with Crohn’s disease, some individuals find that certain foods can trigger symptoms. Get in touch with a certified dietitian who can assist in pinpointing foods that may cause reactions and creating a customized dietary plan.
- Regular exercise: Regular physical activity can help manage symptoms, reduce stress, and promote overall well-being.
- Support groups: Joining support groups or seeking therapy can provide emotional support and help individuals cope with the challenges of living with Crohn’s disease.
It is important to discuss any lifestyle adjustments or home remedies with healthcare professionals to ensure they are appropriate for individual circumstances and do not interfere with prescribed treatments.
Dietary Considerations
The management of Crohn’s disease heavily relies on the importance of maintaining a proper diet. While there is no one-size-fits-all diet for everyone with Crohn’s, certain dietary considerations can help alleviate symptoms and promote overall gut health.
- Enteral nutrition: In some cases, a healthcare professional may recommend enteral nutrition, a form of nutrition that involves consuming specially formulated liquid meals or supplements. This can help reduce inflammation and promote healing in the digestive tract.
- Special diet: Working with a registered dietitian can help develop a personalized diet plan tailored to individual needs and preferences. This may involve avoiding trigger foods, incorporating easily digestible foods, and ensuring adequate nutrient intake.
- Dietary fibers: High-fiber foods may exacerbate symptoms in some individuals with Crohn’s disease. It may be necessary to limit or avoid foods high in dietary fiber, such as whole grains, raw fruits, and vegetables.
- Food diary: Maintaining a food diary and collaborating with a certified dietitian can assist in pinpointing foods that may cause reactions and creating a customized dietary plan.
It is important to work closely with a healthcare professional or registered dietitian to develop a dietary plan that suits individual needs and supports overall health.
Stress Management Techniques
People who suffer from Crohn’s disease may find that stress makes their symptoms worse and even sets off flare-ups. Therefore, incorporating stress management techniques into daily life can be beneficial in managing the condition. Here are some stress management techniques that may help:
- Stress reduction: Identifying and addressing sources of stress can help reduce symptom severity and frequency. This may involve making lifestyle changes, setting boundaries, or seeking support from a mental health professional.
- Relaxation techniques: Reduce stress and improve your health by making time each week to practice relaxation techniques like yoga, meditation, or deep breathing.
- Exercise: Engaging in regular physical activity has been shown to reduce stress levels and improve mood. It is important to choose activities that are enjoyable and appropriate for individual fitness levels.
- Support groups: Connecting with others who are going through similar experiences can provide emotional support and helpful coping strategies. Joining support groups or seeking therapy can be beneficial in managing the challenges of living with Crohn’s disease.
By incorporating these stress management techniques into daily life, individuals with Crohn’s disease can better manage their condition and improve their overall well-being.
Managing Crohn’s Disease through Proper Nutrition
When it comes to Crohn’s disease and general health, good nutrition is extremely important. Individuals with Crohn’s disease often experience nutritional deficiencies and malnutrition due to inflammation and poor absorption of nutrients. Here are some key aspects of nutrition in managing Crohn’s disease.
Recommended Foods
A healthy and balanced diet is crucial for individuals with Crohn’s disease to manage symptoms and support overall health. While specific dietary recommendations may vary depending on individual needs and tolerances, here are some foods that are generally recommended:
- Nutritional foods: Consuming a balanced diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats can help provide essential nutrients and support overall health.
- Anti-inflammatory foods: Foods with anti-inflammatory properties, such as fatty fish (salmon, mackerel), olive oil, nuts, and leafy greens, may help reduce inflammation in the body.
- Hydration: Staying well-hydrated is important for maintaining digestive health and preventing dehydration. Make sure to stay hydrated all day long by drinking plenty of water.
- Dietary supplements: In some cases, dietary supplements may be recommended to address nutrient deficiencies. To ascertain the necessity of supplements, it is advisable to get advice from a healthcare provider or a certified dietician.
By focusing on nutrition and maintaining a healthy diet, individuals with Crohn’s disease can support their overall well-being and manage their condition more effectively.
Foods to Avoid
While there is no one-size-fits-all list of foods to avoid for individuals with Crohn’s disease, certain foods may trigger symptoms or worsen inflammation in some individuals. Here are some common foods that may be problematic:
- Trigger foods: Pay attention to any foods that consistently worsen symptoms or trigger flare-ups. There can be variations from one individual to another.
- Lactose intolerance: Some individuals with Crohn’s disease may also have lactose intolerance, which means they have difficulty digesting lactose, a sugar found in dairy products.
- Non-soluble fiber: Foods high in non-soluble fiber, such as whole grains, raw fruits, and vegetables, may be difficult to digest and can aggravate symptoms for some individuals.
- Spicy foods: Spicy foods, such as chili peppers and hot sauces, can irritate the digestive tract and worsen symptoms in some individuals.
It is important to listen to your body and keep a food diary to identify specific trigger foods. Working with a healthcare professional or registered dietitian can help develop an individualized dietary plan that avoids problematic foods while meeting nutritional needs.
Conclusion
Managing Crohn’s disease effectively requires a comprehensive approach. From understanding the symptoms to exploring treatment options and making lifestyle adjustments, a holistic strategy is key.
Medication, surgical interventions, and emerging therapies play crucial roles in alleviating symptoms. Lifestyle changes, including dietary considerations and stress management, can also make a significant impact.
Remember, regular follow-ups and open communication with your healthcare provider are essential for tailored care.
Make an Appointment
If you are seeking specialized care for Crohn’s disease, you can make an appointment with Dr. Valeria Simone MD, at Southlake General Surgery in Texas, USA.
Dr. Simone is a recognized expert in the field of Crohn’s disease. With her expertise and experience, she can provide comprehensive evaluation, diagnosis, and treatment options tailored to everyone’s needs.
To schedule an appointment, please call +1 (817) 748-0200. Seeking specialized care is essential for the effective management of Crohn’s disease and improving quality of life.
Frequently Asked Questions
What is the best diet for Crohn’s disease?
The best diet for Crohn’s disease varies from person to person, as individual tolerances and preferences differ. Working with a registered dietitian is crucial in developing a personalized diet plan that meets individual nutritional needs and helps manage inflammation and symptoms.
How often should I follow up with my doctor?
The frequency of follow-up visits with a healthcare provider depends on the severity of Crohn’s disease, the frequency of flare-ups, and the effectiveness of the current treatment plan. It is important to work closely with a healthcare provider to determine the appropriate follow-up schedule and make any necessary treatment adjustments.
Can Crohn’s disease be cured?
Currently, there is no recognized cure for Crohn’s disease. However, with appropriate treatment and management, many individuals with Crohn’s disease can achieve remission, in which symptoms are significantly reduced or eliminated. Ongoing research is focused on developing more effective treatment options and understanding the underlying causes of Crohn’s disease.
Do you know about any recent developments in the treatment of Crohn’s disease?
There have been significant advancements in the treatment of Crohn’s disease, particularly in the development of biologic medications that target specific proteins involved in the immune response. Additionally, ongoing clinical trials are exploring new treatment options, such as stem cell therapy and small molecules, to further improve outcomes for individuals with Crohn’s disease.
Medically Reviewed By: Dr. Valeria Simone MD
Board-certified General Surgeon at Southlake General Surgery, Texas, USA.
Follow us on Facebook and YouTube.
References:
- Honap, Sailish, et al. “Anti-Mycobacterium paratuberculosis (MAP) therapy for Crohn’s disease: an overview and update.” Frontline Gastroenterology, vol. 12, no. 5, July 2020, pp. 397–403. https://doi.org/10.1136/flgastro-2020-101471.
- Kuenzig, M. Ellen, et al. “Life expectancy and health-adjusted life expectancy in people with inflammatory bowel disease.” CMAJ. Canadian Medical Association Journal, vol. 192, no. 45, Nov. 2020, pp. E1394–402. https://doi.org/10.1503/cmaj.190976.
- —. “Life expectancy and health-adjusted life expectancy in people with inflammatory bowel disease.” CMAJ. Canadian Medical Association Journal, vol. 192, no. 45, Nov. 2020, pp. E1394–402. https://doi.org/10.1503/cmaj.190976.
- Broekman, Mark M. T. J., et al. “More Dose-dependent Side Effects with Mercaptopurine over Azathioprine in IBD Treatment Due to Relatively Higher Dosing.” Inflammatory Bowel Diseases, vol. 23, no. 10, Oct. 2017, pp. 1873–81. https://doi.org/10.1097/mib.0000000000001163.
- Bruscoli, Stefano, et al. “Glucocorticoid Therapy in Inflammatory Bowel Disease: Mechanisms and Clinical Practice.” Frontiers in Immunology, vol. 12, June 2021, https://doi.org/10.3389/fimmu.2021.691480.
- Grazie, Marco Le. “Infliximab is more effective than cyclosporine as a rescue therapy for acute severe ulcerative colitis: a retrospective single-center study.” Annals of Gastroenterology, Jan. 2021, https://doi.org/10.20524/aog.2021.0584.
- Hanauer, Stephen B. “Reviewing the Use of Vedolizumab for the Treatment of Patients With Crohn’s Disease.” PubMed Central (PMC), 1 May 2022, www.ncbi.nlm.nih.gov/pmc/articles/PMC9666817.
- D’Amico, Ferdinando, et al. “Ustekinumab in Crohn’s Disease: New Data for Positioning in Treatment Algorithm.” Journal of Crohn’s and Colitis, vol. 16, no. Supplement_2, Apr. 2022, pp. ii30–41. https://doi.org/10.1093/ecco-jcc/jjac011.
- Agrawal, Gaurav, et al. “Putting Crohn’s on the MAP: Five Common Questions on the Contribution of Mycobacterium avium subspecies paratuberculosis to the Pathophysiology of Crohn’s Disease.” Digestive Diseases and Sciences, vol. 66, no. 2, Oct. 2020, pp. 348–58. https://doi.org/10.1007/s10620-020-06653-0.
- Adalimumab Injection: MedlinePlus Drug Information. medlineplus.gov/druginfo/meds/a603010.html.
- Certolizumab Injection: MedlinePlus Drug Information. medlineplus.gov/druginfo/meds/a608041.html.
- Infliximab Injection: MedlinePlus Drug Information. medlineplus.gov/druginfo/meds/a604023.html.
- Natalizumab Injection: MedlinePlus Drug Information. medlineplus.gov/druginfo/meds/a605006.html.
- Vedolizumab Injection: MedlinePlus Drug Information. medlineplus.gov/druginfo/meds/a614034.html.

