Crohn’s disease and fistula can be challenging, as these complications can cause discomfort, pain, and other symptoms that affect a person’s quality of life.
However, with proper understanding, diagnosis, and treatment, it is possible to manage these complications and improve overall well-being.
Crohn’s disease is an inflammatory bowel disease affecting the digestive tract, causing chronic inflammation and various symptoms.
One of the complications that can arise from Crohn’s disease is the development of fistulas. Fistulas are abnormal tunnels that form between different organs or between an organ and the skin surface.
In the case of Crohn’s disease, fistulas often occur in the anal area but can also occur in other parts of the digestive tract.
This blog will provide important information about Crohn’s disease and fistulas, including their types, symptoms, diagnosis, treatment options, and post-surgical care.
By learning about these topics, individuals with Crohn’s disease and fistula, as well as their loved ones, can gain a better understanding of the condition and make informed decisions about their healthcare.
Key Highlights
- Fistulas are common complications of Crohn’s disease, occurring in up to half of all adults with the condition.
- There are different types of fistula associated with Crohn’s disease, including anal, vaginal, bladder, and bowel fistulas.
- The fistula diagnosis often involves a physical examination and imaging tests such as CT scans, MRIs, and ultrasounds.
- Options for fistulas include medication, such as antibiotics and biologics, as well as surgical procedures like fistulotomy and seton placement.
- Follow-up care after fistula treatment is important to monitor for recurrence and prevent complications.
- Maintaining good control of Crohn’s disease through medication and lifestyle changes can help prevent the development of fistulas.
Understanding Crohn’s Disease and Its Complications

Crohn’s disease is a condition characterized by persistent inflammation in the digestive tract, leading to an inflammatory bowel disease. This is a lifelong condition with no known cure.
The exact cause of Crohn’s disease is unknown, but it is believed to involve a combination of genetic and environmental factors.
Common symptoms of Crohn’s disease include:
- abdominal pain
- diarrhea
- fatigue
- weight loss
In addition to these symptoms, Crohn’s disease can also lead to complications such as fistulas, strictures, abscesses, and bowel obstructions. These complications can significantly impact a person’s quality of life and require proper diagnosis and management.
The Role of Fistula in Crohn’s Disease
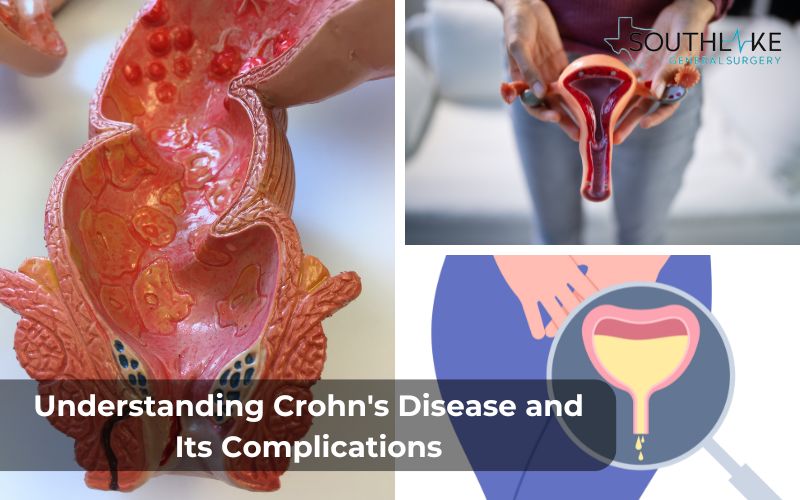
Fistulas are a frequently encountered complication of Crohn’s disease, impacting a significant portion of adults who have this condition. A fistula is an abnormal tunnel that forms between two organs or between an organ and the skin surface.
In the case of Crohn’s disease, fistulas most commonly occur in the anal area, but they can also develop in other parts of the digestive tract.
There are different types of fistulas associated with Crohn’s disease, including anal, vaginal, bladder, and bowel fistulas. The most prevalent kind of fistula is an anal fistula, which develops when a passageway opens between the anus and the skin’s surface, either in the anal canal or the rectum.
Other types of fistulas can connect the vagina to the bladder, rectum, colon, or small intestine, or involve connections between the intestines and the bladder or skin.
The location and severity of a fistula determine the range of symptoms it can cause. These may include pain, swelling, drainage of fluid or stool, and discomfort during bowel movements.
Proper diagnosis and understanding of the type of fistula are essential for effective management and treatment.
Common Symptoms and Early Warning Signs
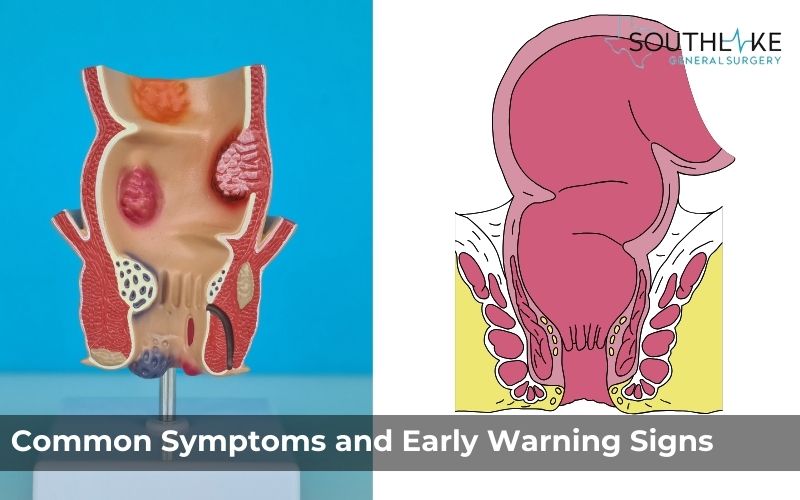
Symptoms of fistula in Crohn’s disease can vary depending on the location and severity of the fistula. Common symptoms include pain, swelling, tenderness, and discomfort in the affected area.
For example, individuals with anal fistulas may experience a tender swelling or lump around the anus that may drain and pain that worsens with movement.
Other symptoms of fistulas can include:
- drainage of fluid
- pus, or stool from the affected area
- redness and inflammation
- discomfort during bowel movements
Some individuals may also experience symptoms related to the organs involved in the fistula, such as urinary tract infections in the case of bladder fistulas.
It’s important to pay attention to these symptoms and seek medical attention if you experience any concerning signs. Early detection and diagnosis of fistulas can lead to more effective treatment and management of Crohn’s disease.
Different Types of Fistulas Associated with Crohn’s Disease
Various types of fistulas can be found in individuals with Crohn’s disease, each manifesting in distinct areas of the body.
- Perianal fistula is a frequently encountered type of fistula that develops between the anal canal or rectum and the surrounding skin near the anus. Symptoms can include swelling, pain, and drainage near the anus.
- Enterovesical fistula, which connects the intestines to the bladder. This can result in symptoms such as urinary tract infections, gas in the urine, and fecal matter in the urine.
- Vaginal fistula can also occur in Crohn’s disease, connecting the vagina to other organs such as the bladder, rectum, colon, or small intestine. Symptoms may include fluid leakage from the vagina, foul-smelling discharge, and urinary or fecal incontinence.
These different types of fistulas require specific treatment approaches and should be diagnosed and managed by a healthcare professional experienced in Crohn’s disease care.
Anal Fistula: Causes and Symptoms
Anal fistulas are the most common type of fistulas that are often linked to Crohn’s disease. They occur when a tunnel forms between the anal canal or rectum and the surface of the skin near the anus. Anal fistulas can cause a range of symptoms, including pain, swelling, tenderness, and discomfort in the anal area.
The exact cause of anal fistula is not fully understood, but they are believed to result from the chronic inflammation and ulceration associated with Crohn’s disease. Fistula formation typically occurs when there is tissue breakdown in the anal canal and the muscles surrounding it.
Individuals with anal fistulas may experience pain that worsens with movement, drainage of fluid or pus from the fistula, and discomfort during bowel movements.
It is important to seek medical attention if you experience these symptoms, as proper diagnosis and treatment are essential for managing anal fistulas in Crohn’s disease.
Enterovesical Fistulas: Bridging the Bowel and Bladder
Enterovesical fistulas can develop when a connection forms between the intestines and the bladder. These fistulas can have various causes, including the chronic inflammation and ulceration associated with Crohn’s disease.
Symptoms of enterovesical fistulas often include:
- urinary tract infections
- gas in the urine
- the detection of fecal matter in the urine.
Individuals may experience an increased frequency of urination and discomfort during urination.
Diagnosis of enterovesical fistulas typically involves:
- a combination of physical examination
- medical history review
- imaging procedures such as computed tomography (CT) scans and ultrasounds
Treatment options may include medication to control inflammation and infection, as well as surgical procedures to repair the fistula and restore normal bladder function.
Early detection and management of enterovesical fistulas are important to prevent complications such as recurrent infections and bladder dysfunction.
Healthcare professionals experienced in Crohn’s disease care can provide guidance and treatment options for individuals with enterovesical fistulas.
Diagnosis and Evaluation of Fistulas in Crohn’s Patients
Diagnosing fistulas in Crohn’s patients involves reviewing medical history, conducting a focused physical examination of the perianal area, and using diagnostic tests like MRI or ultrasound to determine the type and extent of the fistula tract.
Different types vary in symptoms and complexity, necessitating a precise evaluation. While simple cases are easily diagnosed, complex ones require advanced imaging, like CT scans, for accuracy.
The poppy seed test may be used to trace fistula tracts on the skin. Early diagnosis is vital for timely treatment and preventing complications in managing Crohn’s disease.
Advanced Imaging Techniques for Accurate Diagnosis

Advanced imaging techniques play a crucial role in accurately diagnosing fistula related to Crohn’s disease.
- Magnetic resonance imaging (MRI) is commonly employed to visualize fistula tracts, distinguish between simple and complex fistulas, and assess the extent of inflammation.
- CT scans and ultrasounds may also be utilized to provide detailed images of the affected areas.
These imaging modalities help gastroenterologists determine the type of fistula, its relation to surrounding organs, and the best course of treatment.
By combining clinical findings with advanced diagnostic tests, healthcare providers can offer personalized care plans tailored to each patient’s specific needs, improving overall outcomes and quality of life.
Importance of Early Detection in Treatment Success For Crohn’s disease And Fistula

Early detection of fistula in Crohn’s disease is crucial for optimal treatment and care. By identifying and diagnosing fistulas at an earlier stage, healthcare professionals can implement appropriate treatment strategies to prevent further complications and improve outcomes.
Treating fistulas early can help reduce inflammation, prevent infection, and promote healing. Early intervention may involve a combination of medication, such as antibiotics or biologics, to control inflammation and infection, as well as surgical procedures to repair the fistula and restore normal function.
In addition to medical interventions, lifestyle modifications, such as adopting a healthy diet and managing stress, can also play a role in managing Crohn’s disease and fistulas.
Regular follow-up appointments with healthcare professionals are essential to monitor the progress of treatment and make any necessary adjustments based on individual needs and responses.
By emphasizing the importance of early detection and prompt treatment, individuals with Crohn’s disease and fistulas can significantly enhance their overall quality of life and minimize their risk of complications.
Dr. Valeria Simone’s Approach to Treating Crohn’s Disease and Fistula
Dr. Valeria Simone is a renowned healthcare professional specializing in the treatment of Crohn’s disease and fistula. With extensive experience and expertise in gastroenterology and surgery, Dr. Simone takes a comprehensive approach to patient care, focusing on both medical and surgical options.
Dr. Simone understands the importance of personalized treatment plans and tailors medication regimens to suit each patient’s needs. She stays up-to-date with the latest advancements in medical therapies, including biologics and immunomodulators, to provide the most effective treatment options.
When surgical intervention is necessary, Dr. Simone offers a range of minimally invasive techniques for managing fistulas, such as fistulotomy and seton placement.
She emphasizes patient education and ensures patients are well-informed about their treatment options, the benefits and risks of each approach, and what to expect during the recovery process.
With Dr. Simone’s expertise and compassionate care, patients with Crohn’s disease and fistulas can receive comprehensive treatment and management, improving their quality of life and overall well-being.
Tailored Medication Regimens
Medication plays a crucial role in the management of Crohn’s disease and fistulas. Dr. Valeria Simone customizes medication regimens based on each patient’s individual needs and responses.
Biologic medications, such as infliximab, vedolizumab, ustekinumab, and risankizumab, are often used to control inflammation and promote healing in individuals with Crohn’s disease and fistulas.
These medications target specific proteins in the immune system that contribute to inflammation. By blocking these proteins, biologics can help reduce inflammation, alleviate symptoms, and improve overall disease management.
In addition to biologics, immunomodulators like azathioprine and 6-mercaptopurine (6-MP) may be prescribed to modulate the immune response and prevent disease flares. These medications are effective in reducing symptoms and supporting long-term remission.
Dr. Simone closely monitors patients on medication regimens, adjusting doses or medications as needed to optimize treatment outcomes.
By tailoring medication regimens to individual patients, she aims to provide the most effective and personalized care for Crohn’s disease and fistulas.
Minimally Invasive Surgical Options

In cases where surgical intervention is necessary for the treatment of fistulas in Crohn’s disease, Dr. Valeria Simone offers minimally invasive surgical options. These procedures aim to repair the fistula and promote healing while minimizing the impact on surrounding tissues.
One common surgical procedure for fistulas is fistulotomy, a surgical technique that involves cutting open the fistula tract and flattening it out. This procedure can effectively repair fistulas that do not cross the anal sphincter muscles.
Seton placement is another minimally invasive option for managing fistulas. A seton is a thin rubber thread that is placed through the fistula tract to promote drainage and prevent infection. The seton remains in position for several weeks or even months, allowing ample time for the fistula to fully heal.
By offering minimally invasive surgical options, Dr. Simone aims to minimize discomfort, promote faster recovery, and optimize treatment outcomes for individuals with Crohn’s disease and fistulas.
Post-Surgical Care and Recovery Tips

After undergoing surgical treatment for fistulas in Crohn’s disease, proper post-surgical care and recovery are essential for optimal healing and long-term success. Dr. Valeria Simone provides comprehensive guidance and support to help patients navigate this recovery period.
Post-surgical care may involve managing pain and discomfort through prescribed medications and lifestyle modifications. Dr. Simone emphasizes the importance of following post-operative instructions, such as proper wound care, avoiding strenuous activities, and maintaining a healthy diet.
Regular follow-up appointments allow Dr. Simone to monitor the progress of healing, address any concerns or complications, and make any necessary adjustments to the treatment plan.
By providing thorough post-surgical care and recovery tips, Dr. Simone ensures that patients receive the support they need to heal effectively and transition back to their daily activities.
Managing Pain and Preventing Infection
Managing pain and preventing infection are important aspects of post-surgical care for individuals with Crohn’s disease and fistulas. Dr. Valeria Simone provides guidance and support to help patients effectively manage pain and minimize the risk of infection during the recovery period.
Pain management may involve prescribed medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs) or opioids, to alleviate discomfort and promote healing. Dr. Simone works closely with patients to develop personalized pain management strategies based on their individual needs.
Preventing infection is crucial to ensure successful healing. This may involve taking antibiotics for a specific duration, as prescribed by the healthcare professional.
Dr. Simone emphasizes the importance of proper wound care, including keeping the surgical site clean and dry, changing dressings regularly, and following any specific instructions provided.
By actively managing pain and preventing infection, individuals with Crohn’s disease and fistulas can promote optimal healing and reduce the risk of complications during the post-surgical recovery period.
Dietary Adjustments and Lifestyle Changes
Dietary adjustments and lifestyle changes can play a significant role in managing Crohn’s disease and promoting healing after fistula surgery. Dr. Valeria Simone emphasizes the importance of adopting a healthy lifestyle and making appropriate dietary modifications to support overall well-being and recovery.
Dietary adjustments may include avoiding trigger foods that can worsen inflammation and digestive symptoms. Dr. Simone works closely with patients to identify individual dietary triggers and develop personalized nutrition plans to promote healing and prevent flare-ups.
Lifestyle changes can also contribute to improved outcomes. These may include stress management techniques, regular exercise, and adequate hydration to prevent dehydration, which can worsen symptoms and hinder healing.
By making thoughtful dietary adjustments and lifestyle changes, individuals with Crohn’s disease and fistulas can support their overall health, enhance surgical recovery, and reduce the risk of disease flares.
Complications and How to Avoid Them
Complications can arise from Crohn’s disease and fistulas, potentially impacting a person’s quality of life and healing process. Dr. Valeria Simone MD, emphasizes the importance of understanding and addressing potential complications to optimize treatment outcomes and prevent further health issues.
One common complication is the formation of abscesses, which are pockets of pus that can develop around fistulas. These abscesses can cause pain, swelling, and infection. Timely diagnosis and treatment are essential for preventing complications and facilitating the healing process.
Other complications may include delayed healing, recurrence of fistulas, or the development of new fistulas. Close monitoring by healthcare professionals experienced in Crohn’s disease care can help identify and manage these complications effectively.
By taking appropriate preventive measures and addressing complications promptly, individuals with Crohn’s disease and fistulas can minimize the impact on their health and maximize their overall well-being.
Recognizing Signs of Potential Complications
Recognizing the signs of potential complications is crucial for individuals with Crohn’s disease and fistulas. Dr. Valeria Simone emphasizes the importance of being aware of the warning signs and seeking prompt medical attention if any concerning symptoms arise.
Depending on the fistula’s location and severity, the signs of possible complications can differ. These may include increased pain, swelling, redness, or discharge from the affected area. Difficulty with bowel movements, urinary problems, or persistent infections can also indicate complications.
Complications such as abscesses, delayed healing, or the development of new fistulas can significantly impact a person’s quality of life and require appropriate medical intervention.
By being vigilant and proactive in recognizing potential complications, individuals with Crohn’s disease and fistulas can seek timely medical attention and receive the necessary treatment to prevent further complications and promote healing.
When to Seek Immediate Medical Attention
In some cases, immediate medical attention may be required for individuals with Crohn’s disease and fistulas. Dr. Valeria Simone emphasizes the importance of recognizing certain signs or symptoms that may indicate serious complications and warrant urgent medical evaluation.
If you experience severe abdominal pain, high fever, persistent vomiting, or signs of an infection such as worsening redness, swelling, or discharge from the fistula site, it is important to seek immediate medical attention.
These symptoms may indicate abscess formation, severe inflammation, or other serious complications.
A gastroenterologist or specialized healthcare professional experienced in Crohn’s disease care can provide timely evaluation, diagnostics, and appropriate intervention to address these urgent concerns.
By seeking immediate medical attention, when necessary, individuals with Crohn’s disease and fistulas can receive prompt care that can help prevent further complications and optimize treatment outcomes.
Conclusion
Crohn’s disease and fistulas present significant challenges, but with advancements in treatment options and early detection methods, managing and treating these conditions effectively is possible. Seeking timely medical attention and following a personalized treatment plan are crucial for improved outcomes.
By understanding the implications of complications and staying vigilant for warning signs, individuals with Crohn’s disease and fistulas can proactively address their health concerns.
Remember, proactive care and regular consultations with healthcare professionals play a pivotal role in managing these conditions successfully.
Make An Appointment
To schedule an appointment with Dr. Valeria Simone MD, at Southlake General Surgery in Texas, USA, please contact our healthcare expert today at +1 (817) 748-0200.
Offering individualized attention and a variety of cutting-edge treatment options, Dr. Simone is an expert in the field of Crohn’s disease and fistulas.
If you need individualized medical attention, don’t hesitate to get in touch with us. Make the first step towards managing your condition effectively by scheduling a consultation with Dr. Valeria Simone today.
Frequently Asked Questions
How Can Diet Influence Crohn’s Disease and Fistula Management?
Diet can play a significant role in managing Crohn’s disease and supporting healing in individuals with fistulas. A diet low in processed foods, high in fiber, and rich in nutrients can help reduce inflammation, support the immune system, and promote healing.
Working with a registered dietitian experienced in Crohn’s disease can provide personalized dietary recommendations to meet individual needs and support overall health.
How serious is a colon fistula?
Colon fistulas are a significant concern when it comes to Crohn’s disease. Complications such as abscesses, infections, and bowel obstructions may arise. To avoid additional problems and speed up the healing process, it is critical to visit a doctor and get the treatment you need.
What percentage of Crohn’s patients get fistulas?
Fistulas can develop in as many as 50% of adults with Crohn’s disease. The occurrence of fistulas can vary among individuals with Crohn’s disease, and early detection and proper treatment can help prevent complications and promote healing.
What happens if my fistula is untreated?
If a fistula in Crohn’s disease is left untreated, it may lead to complications such as abscess formation, infection, bowel obstruction, or the development of new fistulas. Seeking medical attention and appropriate treatment are crucial to prevent further complications and promote healing.
Can patients with Crohn’s disease successfully undergo surgery to repair fistulas?
Fistulas can be successfully treated surgically for patients suffering from Crohn’s disease. Surgical procedures such as fistulotomy, seton placement, and flap surgery can help repair the fistula, promote healing, and reduce symptoms. However, the appropriate treatment approach may vary depending on the individual’s specific needs and circumstances.
Medically Reviewed By: Dr. Valeria Simone MD
Board-certified General Surgeon at Southlake General Surgery, Texas, USA.
Follow us on Facebook and YouTube.
References:
- Farooqi, Najiha, and Faiz Tuma. “Intestinal Fistula.” StatPearls – NCBI Bookshelf, 17 July 2023, www.ncbi.nlm.nih.gov/books/NBK534208/#:~:text=An%20intestinal%20fistula%20is%20a,the%20intestine%20to%20the%20bladder.
- Young, Calvin, and Kaitryn Campbell. “Biologics versus Immunomodulators or Antibiotics for the Management of Fistulizing Crohn’s Disease: A Review of Comparative Clinical Effectiveness and Cost-Effectiveness.” NCBI Bookshelf, 29 Mar. 2019, www.ncbi.nlm.nih.gov/books/NBK544684.
- Panes, Julian. “Stem Cell Therapy for Perianal Fistulas in Crohn’s Disease.” PubMed Central (PMC), 1 Oct. 2016, www.ncbi.nlm.nih.gov/pmc/articles/PMC5114507.
- Kwon, Eric O., et al. “The Poppy Seed Test for Colovesical Fistula: Big Bang, Little Bucks!” The Journal of Urology, vol. 179, no. 4, Apr. 2008, pp. 1425–27. https://doi.org/10.1016/j.juro.2007.11.085.
- Hashash, Jana G., and Fadi H. Mourad. “Perianal Fistulizing Crohn’s Disease: No Shortcuts to a Deep Understanding of the Disease.” Digestive Diseases and Sciences, vol. 66, no. 5, Aug. 2020, pp. 1392–93. https://doi.org/10.1007/s10620-020-06549-z.
- “Perianal Fistulizing Crohn’s Disease: No Shortcuts to a Deep Understanding of the Disease.” Digestive Diseases and Sciences, vol. 66, no. 5, Aug. 2020, pp. 1392–93. https://doi.org/10.1007/s10620-020-06549-z.
- Nitzan, Orna. “Role of antibiotics for treatment of inflammatory bowel disease.” World Journal of Gastroenterology, vol. 22, no. 3, Jan. 2016, p. 1078. https://doi.org/10.3748/wjg.v22.i3.1078.
- Samaan, Mark, et al. “Biologic therapies for Crohn’s disease: optimising the old and maximising the new.” F1000Research, vol. 8, July 2019, p. 1210. https://doi.org/10.12688/f1000research.18902.1.

