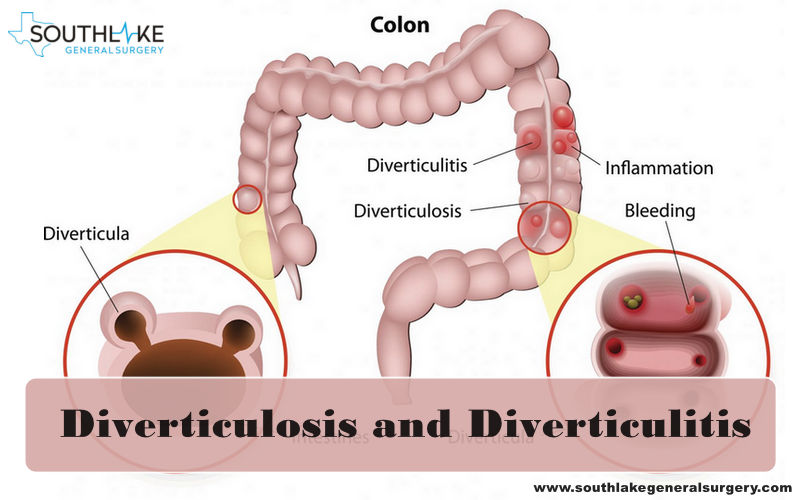
Diverticulitis happens when small pockets in digestive tract, called as diverticula, get inflamed. Diverticula frequently become inflamed once they become infected.
Diverticula are generally found in colon, the largest segment of large intestine. They typically aren’t harmful to digestive system. However, when they become inflamed, they can create pain and different symptoms that can disturb your every-day life.
Who needs diverticulitis surgery?
Diverticulitis surgery is normally performed if diverticulitis is serious or perilous. You can generally deal with your diverticulitis by doing the accompanying:
- taking prescribed antibiotics medicines
- using nonsteroidal anti-inflammatory drugs (NSAIDs), for example ibuprofen
- drinking liquids and avoiding solid meals until symptoms disappear
Doctor may suggest a surgery if you have:
- multiple extreme events of diverticulitis uncontrolled by drugs and way of life changes
- intense pain in abdomen for a a couple of days or more
- constipation, vomiting or diarrhea, that keeps going longer than a couple of days
- a hole or opening in colon (perforation)
- bleeding from rectum
- colon blockage, restricting you from passing waste (bowel obstruction)
- sepsis signs and symptoms
How many types of diverticulitis surgery are there?
The two principle types of surgery for diverticulitis are:
- Bowel resection with primary anastomosis: In this process, surgeon removes any infected or unhealthy colon (called as a colectomy) and suture together the cut closures of the two healthy parts from one or the other side of the formerly infected region (anastomosis).
- Bowel resection with colostomy: In this procedure, surgeon performs a colectomy and joins bowel through an opening in abdomen (colostomy). This opening is known as a stoma. Surgeon may perform a colostomy if there’s an excessive amount of colon inflammation. Contingent on how well you recuperate throughout the following few months, the colostomy might be either transitory or lasting.
Types of Diverticulitis Surgery
- Open: Surgeon makes a six- to eight-inch incision in abdomen to open intestinal location to see.
- Laparoscopic Surgery: Surgeon makes few small incisions and insert a laparoscope which has a small cameras and other surgical instruments into the body through small tubes (trocars) that are normally less than one centimeter in size.
Risk factor in Diverticulitis Surgery
Similarly, as with any surgical procedure, your risk of complexities might be expanded if you:
- are overweight
- are above the age of 60
- are in generally weak health or not receiving enough nutrition
- are going for emergency surgery
- have had diverticulitis surgery or any other abdominal surgery earlier
- have other severe medical conditions like diabetes or high blood pressure
How would I plan for Diverticulitis Surgery?
A few weeks prior your diverticulitis surgery, your surgeon may request you to do the accompanying:
- Stop taking medicines for blood thinning like aspirin or ibuprofen.
- Quit smoking since it makes difficult for your body to heal after surgery.
- Wait until for any existing fever, flu, or cold to break
- Change your diet with fluids and take laxatives to clear bowels.
A day before surgery, you may require to:
- Only take water or clear fluids like clear juice or broth
- Don’t eat or drink anything for at least 12 hours prior the surgery.
- Only take those medicines that your surgeon has prescribed just before surgery.
Ensure you take a break from work or other duties regarding in any event fourteen days to recuperate in the hospital and at home. Have somebody with you to take you home whenever you’re discharged from the hospital.
Treatment of Diverticulitis Surgery at Southlake General Surgery, Texas
To go for a bowel resection with primary anastomosis, surgeon will:
- Make three to five small openings in abdomen (to insert laparoscopy) or make a six-to eight-inches long incision to see intestine and different organs (for open a surgical procedure).
- embed a laparoscope and other special surgical equipment through the incisions (for laparoscopy surgery).
- Fill abdominal area with gas to inflate the abdomen and make room to perform the surgery (for laparoscopy).
- See organs to make ensure there aren’t any other problems.
- Locate the unhealthy part of colon, remove it from the rest of colon, and take it out.
- Suture the two leftover ends of colon back together (primary anastomosis) or open a hole in abdomen and connect the colon to the hole (colostomy).
- Stitch the surgical incisions and clean the areas around them.
Complication of Diverticulitis Surgery
Potential complications of diverticulitis surgery may include:
- blood clots
- infection at surgical site
- hemorrhage (internal bleeding)
- sepsis (an infection all through your body)
- stroke or heart attack
- respiratory failure leading to use of a ventilator for breathing
- heart or kidney failure
- narrowing or blockage of colon from scar tissue
- formation of an ulcer close to the colon (bacteria-infected pus in a wound)
- leaking from location of anastomosis
- close by organs getting injured
- incontinence, or not having the option to control when you pass stool
Recovery after Diverticulitis Surgery
After surgery, you might have to stay in the hospital for about two to seven days. Doctors will continuously observe you and ensure that you pass stools again.
Once you discharge and go home, do the accompanying to help yourself recover:
- Don’t work out, lift heavy objects, or engage in sexual relations for in any event fourteen days after you leave the hospital. Contingent upon your preoperative status and how your surgical procedure went, your primary care physician may suggest this limitation for short or long time.
- Have just clear fluids from initial days. Gradually switch to regular meals as your colon heals or as your primary care physician teaches you to.
- Follow guidelines you were given for dealing with a stoma and colostomy bag.
Takeaway
The viewpoint for diverticulitis surgery is acceptable, particularly if the surgical procedure is performed laparoscopically and you needn’t bother with a stoma.
Consult with your primary care physician immediately if you experience any of the accompanying:
- bleeding from your closed incisions or in your stools
- constipation or diarrhea for more couple of days
- nausea or vomiting
- intense abdominal pain
- fever
You might have the option to have a stoma closed a couple of months after surgical procedure if your colon heals completely. If a large part of colon was eliminated or if there’s a high risk of reinfection, you may have to save a stoma for a long time or forever.
While the reason for diverticulitis is obscure, making healthy way of life changes may check it from creating. Eating a high-fiber meal is one prescribed approach to help forestall diverticulitis.
For more information on causes, symptoms, consultation or surgery on diverticulitis surgery at Southlake General Surgery, Texas. Our healthcare expert will help you to answer all your questions. We are just a call away +1 817-748-0200. Click here to Book an online appointment with us. Top of Form