If you’re researching ‘hysteroscopy,’ you’re likely seeking information on this medical procedure used to examine the inside of the uterus. Hysteroscopy can identify and sometimes treat causes of abnormal bleeding, assist with infertility evaluations, or detect and remove growths like polyps and fibroids.
This article explains the hysteroscopy procedure, its applications, and what you can expect during recovery, ensuring you have the facts you need for informed healthcare decisions.
Key Takeaways
- Hysteroscopy is a minimally invasive diagnostic and therapeutic procedure performed with a hysteroscope to diagnose and treat uterine conditions, such as abnormal bleeding, fibroids, polyps, adhesions, and infertility.
- While diagnostic hysteroscopy is used for visually examining the uterus, operative hysteroscopy involves treating identified issues with specialized tools, often without the need for an overnight hospital stay.
- Though generally safe, hysteroscopy carries risks such as bleeding, infection, and uterine perforation, and recovery may include mild discomfort and cramping, but most patients can resume normal activities quickly, with specific post-procedural precautions advised to prevent complications.
Understanding Hysteroscopy

Hysteroscopy is a procedure enabling a healthcare provider to examine the uterus to diagnose and treat causes of abnormal bleeding. The procedure is performed using something called a hysteroscope, a thin, lighted tube that is inserted into the vagina to examine the cervix and inside of the uterus.
A hysteroscope is a long, slender telescope that is attached to a light source to provide illumination for visualization. It is inserted through the vagina as part of the procedure to diagnose and treat various conditions, including:
- Cervical or endometrial cancer
- Uterine fibroids
- Polyps
- Adhesions
- Abnormal uterine bleeding
- Infertility
Operative hysteroscopy can address abnormal conditions identified during a diagnostic hysteroscopy. It can perform procedures such as polypectomy, myomectomy, and endometrial ablation, which help diagnose and treat uterine fibroids.
The procedure has multiple benefits in the treatment of intrauterine adhesions, such as visually directed lysis and the application of various techniques like cutting, excision with a blunt or sharp instrument, electrocautery, or laser.
This can help remove scar tissue and other adhesions within the uterus, making it a preferred method for the treatment of intrauterine adhesions.
Defining the Procedure
Hysteroscopy involves inserting a slender, flexible thin tube with a camera through the vagina to examine the cervix and uterus, aiding in the accurate diagnosis and treatment of uterine conditions.
This minimally invasive procedure is recommended for patients experiencing abnormal uterine bleeding, especially when periods are longer or heavier than normal, or if there is bleeding between periods. It can help diagnose and treat abnormal growths within the uterus, thus proving to be a very safe procedure for treating uterine conditions.
The distending media in a hysteroscopy procedure serves the purpose of expanding the uterus for improved visualization. This is particularly essential when dealing with uterine conditions such as polyps and fibroids, which are frequently indicated for a hysteroscopy, especially when they cause symptoms such as abnormal bleeding or heavy vaginal bleeding.
This makes the hysteroscopy procedure not only a diagnostic tool but also a therapeutic intervention for a range of uterine conditions.
Diagnostic and Operative Hysteroscopy
While both diagnostic and operative hysteroscopy procedures are used to inspect the inside of the uterus, their applications differ.
Diagnostic hysteroscopy is utilized to identify abnormalities within the uterus. However, when conditions are identified that require intervention, an operative hysteroscopy procedure is executed.
This procedure involves the use of specialized tools to address the conditions once they have been identified. Contrary to what may be assumed, an operative hysteroscopy is not categorized as a major surgical procedure.
Despite the procedure’s ability to treat conditions, it generally does not necessitate an overnight hospital stay, thus making it a convenient option for many women.
Be aware that the type of anesthesia used during a hysteroscopy can range from local to regional or general, depending on the procedure’s specific needs.
Indications for Hysteroscopy
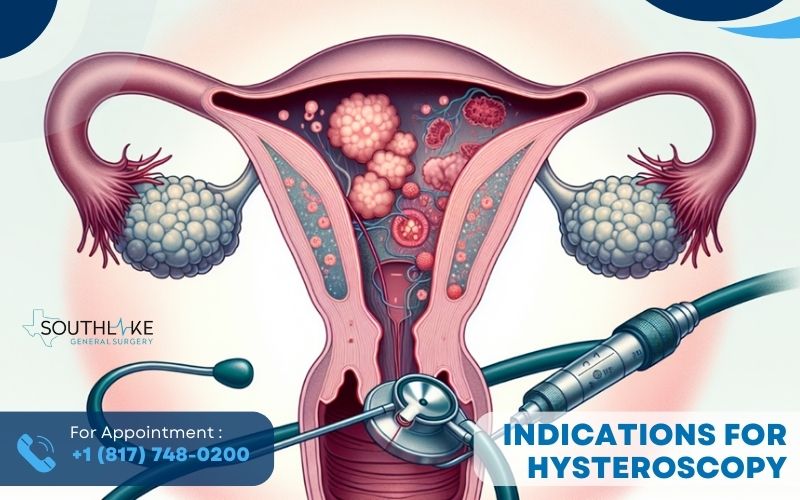
Hysteroscopy is required in various scenarios. It serves to diagnose and treat:
- abnormal uterine bleeding
- uterine fibroids
- polyps
- adhesions
- uterine septum
- endometrial cancer
The procedure can be performed in a hospital setting, at a doctor’s office, or an outpatient surgery center, depending on the preference of the healthcare provider and the specifics of the procedure required.
Local anesthesia, regional anesthesia, or general anesthesia may be administered to patients undergoing a hysteroscopy procedure depending on the requirements of the procedure, thus making it a versatile procedure that can be adjusted according to patient needs.
Moreover, hysteroscopy also plays a significant role in assessing infertility. It is a valuable tool in the evaluation and treatment of conditions that may impact fertility, and health problems such as issues related to the fallopian tubes.
Therefore, a patient should seek medical attention following a hysteroscopy if they encounter abnormal bleeding, severe abdominal pain, or any other worrisome symptoms.
Abnormal Uterine Bleeding and Uterine Conditions
Hysteroscopy has been established as a useful tool in diagnosing and treating abnormal uterine bleeding. Patients undergoing hysteroscopy under local or general anesthesia are advised to empty their bladder and have their vaginal area cleansed with an antiseptic solution.
Additionally, they may be administered medication to aid in relaxation. The procedure performed in hysteroscopy often involves endometrial ablation, which is used to treat abnormal bleeding, especially in cases where other treatments have not been successful.
This procedure has demonstrated high diagnostic precision for endometrial cancer, with an overall sensitivity of 86.4% and a specificity of 99.2%. Diagnostic hysteroscopy, when combined with sonohysterography, has been demonstrated to be up to 88% effective in identifying polyps and submucosal fibroids. This combination can provide valuable diagnostic information for such conditions.
Infertility and Reproductive Concerns
Hysteroscopy also plays a significant role in assessing and treating infertility and reproductive issues. Müllerian anomalies, for instance, refer to abnormalities in the reproductive tract that affect approximately 1-2% of all women, 4% of infertile women, and 10-15% of patients with recurrent miscarriage.
Hysteroscopy is considered the gold standard for diagnosing a septate uterus when conducted alongside laparoscopy, and it is commonly used for:
- Diagnosing and treating uterine polyps
- Removing intrauterine adhesions
- Treating uterine fibroids
- Evaluating and treating endometrial hyperplasia
- Diagnosing and treating uterine septum
The hysteroscopic removal of lesions has been found to not have a negative impact on IVF cycles.
In fact, hysteroscopic polypectomy prior to IUI has been associated with increased odds of pregnancy, with a relative risk of 2.1. However, it is important to keep in mind that myomas only affect a small percentage (1.2–2.4%) of women who are infertile and do not have any other problems.
Also, there are not many controlled studies that show how well hysteroscopic treatment for proximal tubal obstruction works in treating infertility.
The Hysteroscopy Experience

The hysteroscopy process can be divided into three stages: pre-procedure, during the procedure, and post-procedure. Each stage has its own set of expectations and requirements that are important for patients to understand.
In preparation for a hysteroscopy, it is advisable to:
- Schedule the procedure at a non-menstrual time
- Refrain from inserting any vaginal medications, douches, or tampons for 24 hours prior
- Follow any pre-procedure medication or testing instructions given by your physician.
During the procedure of office hysteroscopy, patients may receive local, regional, or general anesthesia, depending on the specific requirements of the procedure.
Pain perception during hysteroscopy can be influenced by factors including the duration of the procedure, parity of the patient, and the patient’s level of anxiety.
The procedure can be performed in a hospital setting or at a doctor’s office, depending on the preference of the healthcare provider and the specifics of the procedure required.
Before the Procedure
Ahead of the procedure, patients can undertake several preparatory steps. For instance, patients are advised to:
- Fast for 6-12 hours before the hysteroscopy if they will be receiving general anesthesia.
- Refrain from using douches, tampons, or vaginal medicines for 24 hours before the procedure.
- Schedule the procedure for a time when they are not menstruating.
- Note that the use of prophylactic antibiotics is not indicated for hysteroscopy.
Further, patients undergoing hysteroscopy under general anesthesia are advised to empty their bladder and have their vaginal area cleansed with an antiseptic. Additionally, they may be administered medication to assist in relaxation.
During the Hysteroscopy Procedure
During the hysteroscopy procedure, the following steps are typically what happens during a hysteroscopy:
- The type of anesthesia – local, regional, or general – is determined based on the specific procedure requirements.
- The hysteroscope is carefully inserted through the cervix into the uterus.
- The uterus is then expanded with liquid or gas to improve visualization.
- The uterine wall is examined for abnormalities.
The average duration of a hysteroscopy procedure can vary from 5 minutes to more than an hour, depending on the specific nature of the procedure. During the procedure, the patient is typically positioned in a dorsal lithotomy position, with her legs placed in adjustable stirrups.
After the Hysteroscopy Procedure
After a hysteroscopy, patients can typically expect the following symptoms:
- Mild discomfort
- Mild cramping
- Light bleeding
- Feeling faint or sick
- Mild fever
Bleeding usually has mild pain that lasts for a few days. It is important to rest and take care of yourself during the recovery period.
Following a hysteroscopy, patients are advised to refrain from douching, sexual intercourse, or inserting any vaginal objects, such as tampons, to facilitate healing and prevent infection.
A patient should seek medical attention following a hysteroscopy if they encounter abnormal bleeding, severe abdominal pain, or any other worrisome symptoms.
Potential Risks and Complications

Though hysteroscopy is generally deemed safe, it carries some risk. Potential risks and complications may include:
- Bleeding
- Infection
- Uterine perforation
- Abnormal placentation
Uterine perforation occurs in approximately 1-1.61% of cases.
Indications of complications subsequent to a hysteroscopy may encompass:
- Profuse bleeding
- Intense pain unresponsive to standard pain relief medication
- Indications of infection such as elevated body temperature, shivering, and malodorous vaginal discharge
- Manifestations of uterine perforation
Managing Complications
When complications occur, their management usually depends on their severity and unique circumstances. For example, minor complications such as minor bleeding can be managed by applying pressure or using medications to promote blood clotting. On the other hand, severe complications such as uterine perforations might necessitate surgical intervention.
In the event of excessive bleeding after a hysteroscopy, it is crucial to promptly seek assessment from the healthcare unit or surgeon. They will evaluate the situation and recommend appropriate treatment and interventions to manage the bleeding, potentially including operative measures for significant bleeding.
Similarly, in the event of a uterine perforation during hysteroscopy, the standard management protocol may involve:
- laparoscopy or laparotomy to address the injury.
- careful observation for symptoms of infection or other problems.
- potential antibiotic treatment.
- in severe cases, an emergent hysterectomy might be necessary.
It is important to follow the guidance of your healthcare provider in these situations.
Recovery and Post-Procedure Care

Post-procedure, patients often feel mild discomfort and need a brief rest period. During the recovery from a hysteroscopy, most patients can resume their daily activities within a brief timeframe, typically within a few hours or days after the procedure.
Following a hysteroscopy, patients are advised to refrain from douching, sexual intercourse, or inserting any vaginal objects, such as tampons, to facilitate the healing of pelvic infection, and prevent infection.
Patients should also be aware of potential sources of discomfort that they may encounter after undergoing hysteroscopy. For example, following a hysteroscopy, a patient can encounter cramping and mild pelvic pain. To address this discomfort, management strategies may involve the use of over-the-counter pain medication and adequate rest.
It is also not advisable for patients to drive immediately after a hysteroscopy procedure. They should arrange for someone else to drive them home, as they may be recovering from anesthesia or experiencing some discomfort.
Returning to Daily Life
After a hysteroscopy, patients should be vigilant for typical indicators of potential complications.
These include heavy bleeding, infection, intrauterine scarring, reaction to anesthesia, and injury to the cervix, uterus, bowel, or bladder.
To manage pain after a hysteroscopy, patients can utilize over-the-counter pain relievers, apply heat, prioritize rest and relaxation, maintain proper hydration, and adhere to post-operative instructions.
In terms of post-procedural precautions, patients are advised to refrain from douching, intercourse, and inserting any vaginal objects, such as tampons, for a specified duration after undergoing a hysteroscopy.
Additionally, it is recommended to avoid lifting heavy objects for 1-2 days post-procedure. Following a hysteroscopy, the typical recovery time is typically a few days, after which most patients can resume their daily routines.
Additional Uses and Considerations
Beyond its primary applications, hysteroscopy can be combined with procedures like laparoscopy for a more holistic assessment and treatment of various reproductive health issues.
Advanced tools, surgical instruments, and energy sources like the VersaPoint system, which utilizes bipolar circuitry for electrosurgery, and a range of fiberoptic lasers are often employed in hysteroscopic surgery.
Specialized tools used in hysteroscopic surgery include the Princess, which is the smallest bipolar resectoscope available, utilized for precision and minimal invasiveness during the procedure.
Hysteroscopy in Conjunction with Other Procedures
Hysteroscopy can be performed simultaneously with other medical procedures, like laparoscopy. This is commonly utilized in cases of unexplained infertility to assess the uterine cavity and cervix.
Conducting hysteroscopy and laparoscopy simultaneously offers the advantage of treating intra-abdominal and intrauterine conditions concurrently.
This combined approach is deemed safe and has demonstrated favorable outcomes in addressing specific conditions, offering a more comprehensive assessment and treatment alternative.
However, while combining hysteroscopy with dilation and curettage (D&C) can yield positive outcomes, potential hazards like uterine perforation exist. Therefore, it’s essential to have a thorough discussion about these with your healthcare provider before proceeding.
Summary
In conclusion, hysteroscopy is a versatile, minimally invasive diagnostic and treatment tool used in gynecology. It is a safe procedure that can be used to treat a wide array of uterine conditions, including abnormal bleeding and infertility.
Although there are potential risks and complications, they are rare and can be effectively managed in most cases. Patients should feel confident that by choosing hysteroscopy, they are opting for a procedure that has been proven to be safe and effective in treating various uterine conditions and addressing fertility concerns.
A Note From Southlake General Surgery – Dr. Valeria Simone MD
As a medical professional specializing in general surgery, I truly value the importance of comprehensive patient education. Understanding your health and the procedures you undergo is crucial for informed decision-making and recovery.
This guide on hysteroscopy aims to provide you with a thorough understanding of the procedure, its benefits, and the recovery process. Remember, your health is your greatest asset, and making informed decisions is a significant part of maintaining it.
Make an Appointment

We understand that health concerns can be a source of anxiety, and we’re here to help. If you’re experiencing any symptoms or have concerns about your reproductive health, don’t hesitate to make an appointment with us.
If you require assistance or direction, our team of professionals is here to help. We’re committed to making your experience as comfortable as possible, from the moment you walk in the door to the time you leave.
Contact us today to schedule your appointment at +1 (817) 748-0200 and you can also make an online appointment with us. Make a positive change for your health by starting now.
Frequently Asked Questions
How painful is hysteroscopy?
Hysteroscopy can be moderately to severely painful for some patients, especially during the passage through the cervical canal. Talking to your doctor about pain management alternatives is essential.
What is a hysteroscopy done for?
A hysteroscopy is done to diagnose and treat the causes of abnormal uterine bleeding, investigate symptoms such as heavy periods, unusual vaginal bleeding, postmenopausal bleeding, pelvic pain, repeated miscarriages, or difficulty getting pregnant, and diagnose conditions such as fibroids and polyps.
Are you put to sleep for a hysteroscopy?
You may receive general anesthesia or a local anesthetic to numb your cervix for a hysteroscopy. Longer or more complex procedures may require general anesthesia and you will be asleep during the operation.
How long does it take to recover from a hysteroscopy?
You can generally expect to go back to most of your normal activities in 1 or 2 days after a hysteroscopy. Some people may even return to work the same day, but it’s advisable to take a day off to recover, especially if you’ve had a general anesthetic.
Why would you need a hysteroscopy?
You may need a hysteroscopy to investigate abnormal bleeding, diagnose infertility or repeated miscarriages, and identify conditions like fibroids and polyps. It can also help investigate symptoms or problems such as heavy periods, unusual vaginal bleeding, postmenopausal bleeding, pelvic pain, and difficulty getting pregnant.
Medically Reviewed By: Dr. Valeria Simone MD
Board-certified General Surgeon at Southlake General Surgery, Texas, USA.
Follow us on Facebook and YouTube.
References:
- Moore, J. F. (2023, July 18). Hysteroscopy. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK564345/
- Elahmedawy, H., & Snook, N. J. (2021, July 1). Complications of operative hysteroscopy: an anaesthetist’s perspective. BJA Education. https://doi.org/10.1016/j.bjae.2021.03.001
- Salazar, C., & Isaacson, K. (2018, February 1). Office Operative Hysteroscopy: An Update. Journal of Minimally Invasive Gynecology. https://doi.org/10.1016/j.jmig.2017.08.009
- Barbieri, E., Kashyap, S., & Chung, P. H. (2010, January 1). Infertility and In Vitro Fertilization. Elsevier eBooks. https://doi.org/10.1016/b978-0-12-374271-1.00035-6
- Vitale, S. G., Carugno, J., Riemma, G., Török, P., Cianci, S., De Franciscis, P., & Parry, J. (2021, April 1). Hysteroscopy for Assessing Fallopian Tubal Obstruction: A Systematic Review and Diagnostic Test Accuracy Meta-analysis. Journal of Minimally Invasive Gynecology. https://doi.org/10.1016/j.jmig.2020.11.013
- Sinha, P., Yadav, N., & Gupta, U. (2017, November 7). Use of Hysteroscopy in Abnormal Uterine Bleeding: An Edge Over Histopathological Examination. The Journal of Obstetrics and Gynecology of India. https://doi.org/10.1007/s13224-017-1065-5