The pancreas is a sizable gland with a shape reminiscent of a tadpole, located deep within the abdominal cavity. It is quite essential for the processes of digestion and the regulation of blood sugar levels in our body.
Diagnosing pancreatic disease can be challenging because of the organ’s positioning. However, there are actions you can take to lower your likelihood of experiencing these issues.
What is a Pancreas?
The pancreas is a big gland located behind your stomach. It resides in the curve of your duodenum, which is the initial segment of your small intestine. Your pancreas functions as a dual organ. Your pancreas serves two primary roles, and it produces:
- Enzymes (amylase, lipase, trypsin) that assist in the digestive process which includes the breakdown of carbohydrates, proteins, and fats (exocrine system).
- Hormones (insulin, glucagon, somatostatin) to regulate the levels of sugar present in your blood (endocrine system).
Function of Pancreas
What role does the pancreas play in our body?
The pancreas is an essential organ that keeps your body in balance and helps support other organs such as your heart, liver, and kidneys.
One of the primary functions of your pancreas is to assist in the digestive process and it is responsible for releasing hormones that help regulate blood sugar levels.
Help with the process of digestion
Your pancreas produces approximately 1-4 liters of enzyme-rich digestive juice daily to help you digest nutrient breakdown from consumed foods. The specific amount can change based on the quantity of food you consume.
Following a meal, it’s likely that you don’t give much thought to the process of digestion unless you experience discomfort or develop indigestion.
However, multiple organs collaborate to assist in the breakdown process. Let’s explore what happens when food enters your stomach:
The Digestive Process: A Step-by-Step Breakdown
- Step 1: Pancreatic Juice Release: After eating, your pancreas releases digestive juice into small ducts that flow into your main pancreatic duct.
- Step 2: Duct Connection: Your main pancreatic duct merges with the bile duct. This duct transports bile from your liver to the gallbladder.
- Step 3: Bile Transport: Bile travels from your gallbladder to the duodenum (small intestine’s first section).
- Step 4: Digestive Breakdown: Pancreatic juice and bile enter the duodenum to breakdown food into nutrients.
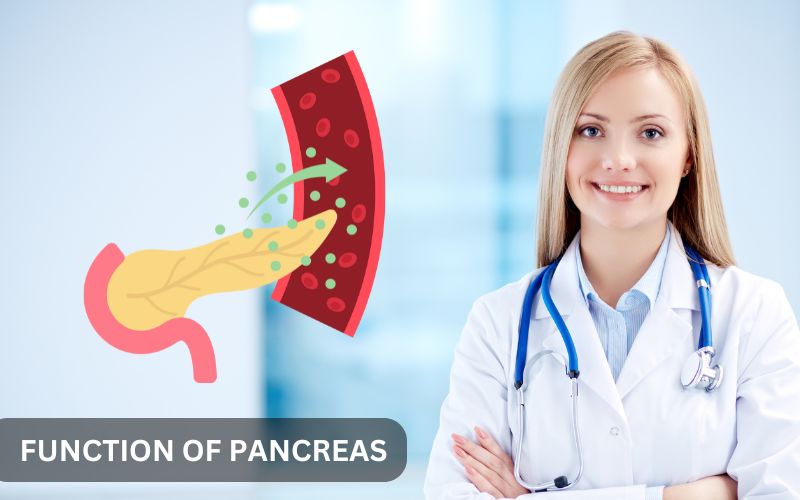
Pancreas Create Hormones

The pancreas produces important hormones, such as insulin and glucagon, which play a crucial role in regulating the sugar levels in your bloodstream.
When your blood sugar levels rise, your pancreas produces insulin to help bring them back down. When the blood sugar levels drop, your pancreas generates glucagon to help raise them back up.
Maintaining balanced blood sugar is essential for your body to function effectively, ensuring that vital organs such as your heart, liver, kidneys, and brain operate smoothly.
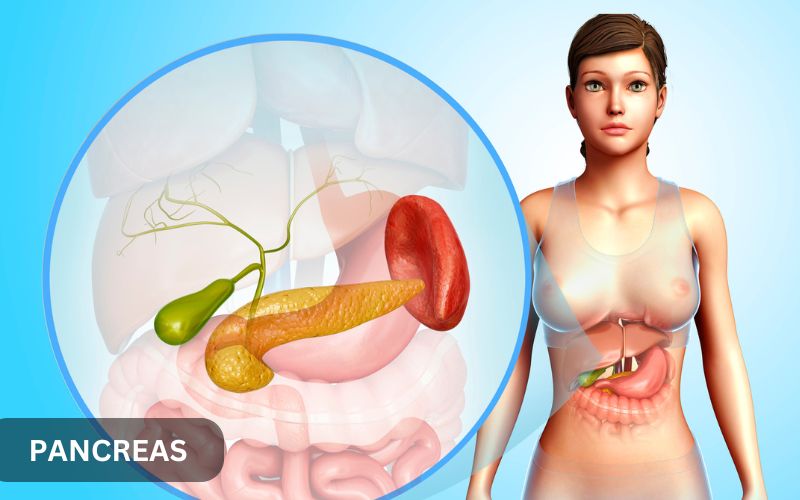
Anatomy of Pancreas
Location of Pancreas in Body
Your pancreas is located deep within your abdomen, positioned behind the stomach and in front of the spine. The spleen, gallbladder, and liver surround the pancreas.
Anatomy of Pancreas
Pancreas has various components, each fulfilling a distinct function.
- Head: The head of the pancreas is located on the right side of the abdomen, which measures about 2-3 centimeters adjacent to the small intestine.
- Body: The pancreas central portion measures about 10-12 centimeters long and it contains most of the pancreatic tissue.
- Tail: The pancreas’ tail is about 2-3 cm in diameter, and it extends to the left side of the abdomen, adjacent to the spleen.
- Pancreatic Duct: The pancreatic duct runs the full length of the pancreas.
How does the pancreas appear?
The pancreas is a glandular organ, that measures about 6-10 inches (15-25 cm) in length and is situated in the abdominal cavity.
Your pancreas has a unique shape that resembles a tadpole, featuring a thicker head and a thin tail. Its surface is uneven, resembling the texture of a corn cob.
The pancreas constitutes around 0.1-0.2% of total body mass, which is roughly the weight of a small banana.
Common Pancreatic Disorders and Symptoms

The pancreas is tucked away in your body, but it can still face issues. These issues can go from short-term inflammation of the pancreas to lasting illnesses.
Which diseases and disorders can compromise the pancreas?
Your pancreas can be affected by various conditions and ailments that can influence its functionality, including:
- Chronic pancreatitis is persistent inflammation. It occurs due to excessive alcohol consumption, which may lead to discomfort, digestive issues, and the onset of diabetes.
- Pancreatic cancer is a serious condition, and it is hard to detect in the early stages. It can also spread to other organs before being noticed. Signs and symptoms of pancreatic cancer may include pain in the abdominal area or back, weight loss, and jaundice.
- Pancreatic cysts are quite common among individuals. They are fluid-filled sacs that could potentially contain precancerous cells. Regular checks and tests, like endoscopic ultrasound and biopsy, are important to keep an eye on these cysts.
- Type 1 diabetes occurs when the pancreas is unable to generate adequate insulin levels.
- Type 2 diabetes happens when the body makes insulin but does not use it well.
- Hypoglycemia (low blood sugar) happens when blood glucose levels drop under 70 mg/dL, which can pose risks to the brain and essential organs. It is typically associated with diabetes, yet it can also impact individuals who do not have the condition.
- Hyperglycemia (high blood sugar) arises when blood sugar levels exceed 180 mg/dL, which can lead to harm to organs and tissues. This situation frequently arises in diabetes when there is an insufficient amount of insulin available. If left unaddressed, it may lead to significant complications such as diabetic ketoacidosis.
Symptoms of Pancreatic Disease
Diseases that impact the pancreas can have strange symptoms. This can make it difficult to spot them early. It’s very important to recognize the warning signs. If you observe any of these signs, it is recommended to consult a physician.
Digestive Symptoms may include:
- Abdominal pain (upper or middle)
- Nausea and vomiting
- Diarrhea or oily stools
- Weight loss
- Loss of appetite
Pancreatitis-Specific Symptoms:
- Sudden, severe abdominal pain
- Fever
- Swollen abdomen
- Tenderness to the touch
Diabetes-Related Symptoms (due to insulin imbalance):
- Increased thirst and urination
- Fatigue
- Blurred vision
- Slow healing wounds
Other Symptoms:
- Jaundice (yellowing skin and eyes)
- Dark urine
- Pale or greasy stools
- Indigestion
- Bloating
Severe Symptoms (seek immediate medical attention):
- Severe abdominal pain
- Vomiting blood
- Bloody stools
- Difficulty breathing
- Rapid heartbeat
Diagnostic Approaches to Evaluate the Health of the Pancreas

To assess the functionality of your pancreas, healthcare professionals typically start by reviewing your medical history and conducting a physical examination.
To identify issues, physicians might require specific assessments that may include:
Imaging Tests:
- Computed Tomography (CT) scan
- Magnetic Resonance Imaging (MRI)
- Ultrasound (US)
- Endoscopic Ultrasound (EUS)
- Positron Emission Tomography (PET) scan
Blood Tests:
- Amylase and lipase levels (pancreatitis)
- Glucose tolerance test (diabetes)
- Pancreatic enzyme tests (elastase, trypsin)
- Tumor marker tests (CA 19-9)
Endoscopic Procedures:
- Endoscopic Retrograde Cholangiopancreatography (ERCP)
- Endoscopic Ultrasound (EUS)
- Pancreatoscopy
Pancreatic Function Tests:
- Pancreatic stimulation test (measures enzyme secretion)
- Glucose tolerance test (assesses insulin function)
Biopsy and Histopathology:
- Fine-needle aspiration biopsy (FNAB)
- Core needle biopsy
Other Tests:
- Stool tests (elastase, fat content)
- Pancreatic juice analysis
- Genetic testing (hereditary conditions)
Treatment Options: From Medication to Surgery
Treatment for pancreatic diseases varies depending on the condition, how far it has progressed, and the person’s health. Your healthcare providers address pancreatic conditions through various approaches, tailored to the specific condition at hand.
Treatment Options by Condition:
- Diabetes: Insulin replacement therapy
- Pancreatic Cancer: Chemotherapy, radiation therapy, and surgery
- Pancreatitis: Dietary modifications, medications, and surgery (in severe cases)
- Advanced Cases: Pancreas transplant or pancreatectomy (partial/total removal)
Islet Cell Transplant: Transplanting islets of Langerhans cells into the liver
Medication for pancreatic treatment
There are several medications available that can help in managing pancreatic conditions:
- Pain management: analgesics, narcotics
- Pancreatitis: anti-inflammatory medications
- Diabetes: oral hypoglycemics, insulin
- Enzyme replacement: pancreatic enzymes
- Antibiotics (infections)
Surgical Treatment for Pancreatic Conditions
In many cases, surgical procedures are essential for addressing pancreatic issues, serving either as the main approach or alongside additional treatment methods. The objective of surgical intervention is to eliminate unhealthy tissue, alleviate symptoms, and enhance overall quality of life.
Various procedures are employed, depending on the condition’s severity and location.
- Pancreatectomy, involving partial or total removal of the pancreas, is commonly performed for pancreatic cancer, severe chronic pancreatitis, and benign tumors.
- The Whipple procedure, a complex operation removing the head of the pancreas, duodenum, bile duct, and gallbladder, is generally reserved for pancreatic cancer and ampullary cancer.
- Distal pancreatectomy, involves the surgical removal of the body and tail of the pancreas, serving as a treatment option for pancreatic cancer, benign tumors, and cysts.
- Pancreas transplantation, either alone or simultaneously with kidney transplantation, offers a treatment option for severe type 1 diabetes and end-stage renal disease.
- Islet cell transplantation, involving the transfer of insulin-producing cells into the liver, provides an alternative for managing severe type 1 diabetes and chronic pancreatitis.
- Necrosectomy, the removal of dead pancreatic tissue, is performed in cases of severe acute pancreatitis or infected pancreatic necrosis.
Surgical approaches include open surgery, laparoscopic surgery, and robotic-assisted methods, each with varying benefits and risks. It’s important to consult with a qualified healthcare professional to find the best surgical approach tailored to your specific pancreatic condition.
The Role of Diet and Lifestyle in Managing Pancreatic Health

Maintaining good health for your pancreas is not only about treatment. It is also about preventing problems and taking charge of your health. A nutritious diet plays a crucial role in this context.
Dietary Recommendations:
- Low-Fat Diet: Reduce fat intake to minimize pancreatic strain.
- High-Fiber Diet: Include fruits, vegetables, and whole grains in your daily meals.
- Hydration: Drink plenty of water every day to keep yourself hydrated.
- Avoid Trigger Foods: Limit or avoid spicy, fatty, or high-sugar foods that may create complications.
- Pancreatic-Friendly Foods: Include lean proteins, low-fat dairy, and omega-3 rich foods.
Lifestyle Modifications:
- Quit Smoking: It reduces the risk of pancreatic cancer and other pancreatic disease progressions.
- Limit Alcohol: Avoid excessive alcohol consumption.
- Exercise Regularly: Promote weight management and insulin sensitivity.
- Stress Management: Participate in relaxation techniques such as meditation or yoga.
- Maintain Healthy Weight: This will help reduce the risk of pancreatic disease.
- Sufficient Sleep: Aim for 7-8 hours of sleep.
Nutritional Considerations for Pancreas Health:
- Pancreatic Enzymes: You can take supplements with amylase, lipase, and trypsin on your doctor’s recommendation.
- Vitamin D: This will maintain adequate levels.
- Antioxidants: Include vitamins C and E, and beta-carotene.
- Omega-3 Fatty Acids: Found in fatty fish, and flaxseeds.
Importance of Regular Check-Ups and Early Diagnosis
- Find any issues with your pancreas early.
- Check for signs of possible pancreatic disease.
- Offer help before symptoms get worse.
- Make sure you stay healthy.
- Check how healthy you are overall.
- Look for risk factors for pancreatic diseases.
- Find any early signs you might miss.
Finding problems early can really help improve treatment for pancreatic conditions. This is especially true for pancreatic cancer.
Many people find out they have pancreatic cancer at later stages, which is not good for getting treatment. However, if doctors find precancerous cells or early tumors, the chances for successful treatment are much higher.
If you have symptoms that might mean pancreatic cancer and can’t find a reason for them, you should visit a doctor soon. Pay attention to signs like pain in your stomach or back, weight loss that is not explained, yellowing of the skin or eyes (jaundice), not feeling hungry, or changes in your bathroom habits.
Conclusion
The pancreas is essential for maintaining the overall well-being of our body. It generates enzymes for digestion and assists in regulating blood glucose levels. Your pancreas is essential for both digestion and hormone regulation in the body. Issues related to the pancreas, such as inflammation or cancer, can result in significant health complications.
It is very important to know the signs and risk factors of pancreatic problems. To keep your pancreas healthy, you should eat a balanced diet, have regular doctor visits, and ask for medical help quickly if you notice any worrying symptoms.
Taking care of your pancreas is important for a healthy and happy life. Choose wisely to protect your pancreatic health.
Make an Appointment
To book your appointment with Dr. Valeria Simone, MD, at Southlake General Surgery in Texas, USA, call +1 (817) 748-0200. Dr. Simone helps with pancreatic health. She works on problems like pancreatic cancer, issues in the digestive system, and pancreatic enzymes.
If you need help with blood sugar or think you might have problems with your pancreas, Dr. Simone can assist you. Common signs include abdominal pain and weight loss. Contact us today to begin looking after your pancreatic health.
Frequently Asked Questions
Can lifestyle changes minimize the risk of pancreatic diseases?
Making healthy choices is very important. Eating a balanced diet is key. Exercising regularly matters as well. It’s also important to avoid smoking. When you make these changes, you can lower the risk factors for many pancreatic diseases. This can also help keep your pancreas healthy.
What are the early signs of pancreatic problems?
- Early signs that there may be issues with the pancreas can include:
- Constant abdominal pain that might reach the back
- Unexplained weight loss
- Jaundice occurs when there is a yellowing of the skin or eyes.
- Changes in stool color
- Problems with digestion
Can one live without a pancreas?
Life can be hard without a pancreas, but you can make it work with the right care. Diabetes management is a lifelong commitment. This includes using insulin. You might also need to take enzyme supplements for better digestion. Additionally, hormone replacement therapy can help you feel good each day.
Medically Reviewed By: Dr. Valeria Simone MD
Board-certified General Surgeon at Southlake General Surgery, Texas, USA.
Follow us on Facebook and YouTube.
References:
- Hariharan, D., Saied, A., & Kocher, H. (2008). Analysis of mortality rates for pancreatic cancer across the world. HPB, 10(1), 58–62. https://doi.org/10.1080/13651820701883148
- Karamanou, M. (2016). Milestones in the history of diabetes mellitus: The main contributors. World Journal of Diabetes, 7(1), 1. https://doi.org/10.4239/wjd.v7.i1.1
- Noh, T., Lee, S. E., & Park, J. (2012). Laparoscopic treatment of annular pancreas in adults: report of a case. Korean Journal of Hepato-Biliary-Pancreatic Surgery, 16(1), 43. https://doi.org/10.14701/kjhbps.2012.16.1.43
- Shahid, Z., & Singh, G. (2022, October 3). Physiology, Islets of Langerhans. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK542302/
- Mohammed S, Van Buren G 2nd, Fisher WE. Pancreatic cancer: advances in treatment. World J Gastroenterol. 2014 Jul 28;20(28):9354-60. doi: 10.3748/wjg.v20.i28.9354. PMID: 25071330; PMCID: PMC4110567.
- Institute for Quality and Efficiency in Health Care (IQWiG). (2021, May 25). Acute pancreatitis: Learn More – How is acute pancreatitis treated? InformedHealth.org – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK298835/
- Bishop, M. A., & Simo, K. (2023, June 21). Pancreatectomy. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK564309/