Small intestine resection surgery is a crucial procedure that involves removing a diseased segment of the intestine. Patients undergo this surgical procedure to treat illnesses such as Crohn’s disease or colorectal cancer. General anesthesia is commonly administered to provide a painless procedure.
The goals of the surgery include symptom relief and an overall improvement in the patient’s well-being. Understanding the post-surgery process and knowing what to anticipate is crucial in ensuring a smooth and successful recovery.
This introduction provides the necessary groundwork for understanding the complexities of small intestinal resection surgery.
Key Highlights
- Small intestine resection surgery is performed to treat conditions like colorectal cancer, Crohn’s disease, and short bowel syndrome.
- Symptoms indicating the need for surgery include bowel obstruction, persistent pain, and complications from underlying bowel diseases.
- The diagnosis process involves blood tests and consultations with a healthcare team to determine the necessity of surgery.
- Different types of resection surgeries, such as segmental and total bowel resections, are tailored to individual patient needs.
- Preparing for surgery includes pre-operative assessments, dietary modifications, and an understanding of surgical techniques like open and laparoscopic surgery.
- Post-surgery care focuses on immediate recovery, long-term dietary adjustments, managing potential complications, and maintaining quality of life post-resection.
The Need for Small Intestine Resection Surgery

Small intestine resection surgery may be necessary in cases where the proper functioning of the intestine is compromised due to conditions such as Crohn’s disease or bowel obstruction.
Symptoms such as severe ulcers or regional enteritis may necessitate this type of surgery to improve the patient’s quality of life. Diagnosing these issues through blood tests or imaging helps determine the extent of the resection needed.
Once identified, surgical intervention becomes crucial to alleviate symptoms and prevent complications, with the ultimate goal of restoring the intestine’s normal function.
Identifying Symptoms and Conditions Leading to Surgery

Symptoms and conditions necessitating small intestine resection surgery include:
- Bowel obstruction
- Severe ulcers
- Crohn’s disease
- Colorectal cancer
If you experience persistent pain, blood in stools, or bloating, consult a doctor. Diagnostic tests like blood tests, imaging scans, and endoscopy help pinpoint the issue.
Your healthcare team will determine if surgery is the best option based on the findings. For prompt action and treatment, it is critical to quickly identify these signs.
Understanding the Diagnosis Process
Diagnosis for small intestine resection involves various steps to determine the precise condition. From detailed physical exams to imaging tests like CT scans or MRIs, the healthcare team aims to identify the specific issues prompting surgery.
Blood tests can reveal crucial information about your small bowel health, while procedures like endoscopy provide direct visual inspections.
Understanding the diagnosis process is fundamental for establishing the necessity and extent of resection surgery and ensuring appropriate treatment plans align with your specific condition.
Different Types of Small Intestine Resections
Segmental resection involves removing part of the small intestine, often performed for localized issues like tumors. Total small bowel resection is more extensive, addressing conditions spread throughout the organ, such as severe Crohn’s disease.
Both procedures aim to improve the patient’s health by eliminating diseased portions and reconnecting the healthy ends of the intestine. Understanding these distinctions is crucial for patients facing small intestine surgery.
Segmental Resection: What It Involves
Segmental resection is a surgical procedure that entails the removal of a specific portion of the intestine that has been damaged by conditions such as Crohn’s disease or colorectal cancer.
During the procedure, the surgeon removes the parts of the intestine that are affected by illness and then joins together the remaining healthy ends of the intestine.
This type of surgery aims to alleviate symptoms and prevent complications such as bowel obstruction.
The healthcare team carefully assesses the extent of resection required to ensure optimal outcomes. Understanding what segmental resection involves can help patients prepare mentally for the surgical procedure and recovery process.
Total Small Bowel Resection: When It’s Necessary
Total small bowel resection becomes necessary in cases where extensive damage or disease affects large portions of the small intestine, such as in advanced Crohn’s disease or severe bowel obstructions.
This type of surgery aims to remove the diseased segment and preserve as much healthy intestine as possible to maintain proper digestive function.
Your healthcare team will recommend this procedure when other treatment options have been exhausted, and the remaining intestine cannot adequately absorb nutrients or allow for normal bowel function.
Preparing for Your Surgery
Discussion with your healthcare team regarding pre-operative assessments and necessary tests is vital before your small intestine resection surgery.
- Dietary modifications and lifestyle adjustments preceding the procedure are crucial for optimal outcomes.
- Following guidelines for clear liquids and appropriate fluid intake is essential.
- Being mentally prepared for the surgery and understanding the upcoming changes will contribute to a smoother recovery process.
- Compliance with pre-operative instructions ensures a successful surgical experience.
Pre-operative Assessments and Tests
Prior to small intestine resection surgery, various pre-operative assessments and tests are conducted to ensure optimal surgical outcomes. These assessments may include blood tests to assess your overall health status and suitability for surgery.
Imaging studies, such as CT scans or MRIs, may be performed to visualize the affected areas of the intestine. Your healthcare team might also require other tests to evaluate specific conditions, like Crohn’s disease or colorectal cancer.
These evaluations are essential for strategizing the surgical process and minimizing risks.
Dietary and Lifestyle Changes Before Surgery
Before undergoing resection of the small intestine, it’s crucial to make necessary dietary and lifestyle adjustments. The day before surgery, your healthcare staff may advise you to drink only clear liquids or go on a liquid diet to make sure your intestines are clean.
Staying hydrated by drinking plenty of water and following specific instructions regarding food intake is essential.
Making these adjustments will better prepare your body for the surgery and facilitate a speedier recovery. Following guidance from your healthcare team is vital for optimal results.
Surgical Techniques Explained
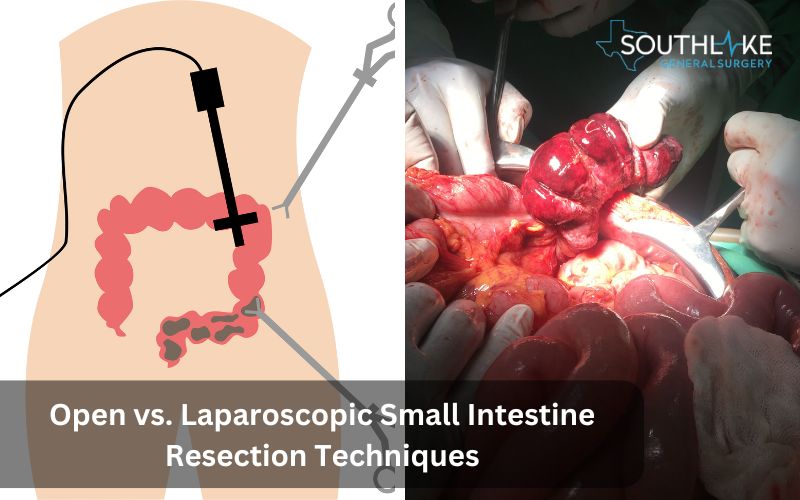
During small intestine resection surgery, two primary techniques are commonly used: open surgery and laparoscopic surgery. One large incision is all that’s needed to gain access to the surgical site during open surgery.
Laparoscopic surgery, on the other hand, is minimally invasive since it uses a series of tiny incisions to introduce a camera and surgical instruments. The advantages of laparoscopic surgery over open surgery include shorter recovery times, less discomfort, and less scars.
Your healthcare team will recommend the most suitable technique based on your specific condition.
Open Resection Surgery: Procedure and Expectations
During open resection surgery, a large incision is made in the abdomen to access and remove the diseased part of the small intestine.
This traditional surgical approach allows the healthcare team to directly visualize and work on the affected area. For your comfort throughout the procedure, general anesthesia is administered.
Expect a longer recovery time compared to laparoscopic surgery, as the open technique involves more extensive tissue manipulation and a larger incision.
Clear communication with your healthcare team about post-operative expectations is key for a smoother recovery process.
Laparoscopic Resection: Benefits and Considerations
Laparoscopic resection is an alternative to open surgery that is safer, less invasive and requires less time to recover from. The technique utilizes surgical tools and a camera to operate through small cuts, minimizing damage to nearby organs.
This method often helps patients feel less pain and scars. However, considerations include the complexity of the procedure and the need for expertise in using the laparoscopic technique.
Discuss with your healthcare team to determine if laparoscopic resection is suitable for your small intestine surgery.
Post-Surgery: Recovery and Rehabilitation

After small intestine resection surgery, the focus shifts to post-operative recovery and rehabilitation. Immediate care involves monitoring for complications, ensuring proper wound care, and initiating mobility.
Long-term recovery emphasizes transitioning from liquid to solid foods gradually, adjusting activity levels based on medical advice, and attending follow-up appointments to track progress.
Patients may experience temporary discomfort, but managing pain effectively enables a smoother recovery process. Adhering to dietary guidelines and gradually increasing activity levels are key to a successful recuperation.
Communication with doctors is essential for post-surgery success.
Immediate Post-operative Care
Following small intestine resection surgery, immediate post-operative care is crucial. Patients are closely monitored for any signs of complications, such as infection or abnormal bleeding.
- Pain management is carefully addressed to ensure patient comfort.
- Intravenous fluids may be administered to maintain hydration, and the healthcare team monitors the return of bowel function.
- Early mobilization is encouraged to prevent blood clots and promote faster recovery.
- Patient education on wound care, activity restrictions, and medication management is provided to facilitate a smooth transition into the recovery phase.
Long-term Recovery: Diet and Activity Adjustments
After small intestine resection surgery, long-term recovery involves crucial diet and activity adjustments.
- Following your healthcare team’s guidance is essential to ensure you regain strength and maintain overall well-being.
- To aid in the healing of your intestines, begin with nutrient-rich liquids and work your way up to solid foods.
- Adequate hydration and carefully monitored physical activity play significant roles in your recovery process.
- Balancing rest and movement is key to avoiding complications and enhancing your long-term health outcomes.
Potential Complications and How They Are Managed

Post small intestine resection surgery, several complications may arise, including infections, blood clots, or bowel obstructions.
- Infections are typically managed with antibiotics; blood clots may require blood thinners or compression stockings.
- Bowel obstructions might need further surgery or non-surgical interventions like a nasogastric tube.
Notify your healthcare team promptly if you experience persistent pain, fever, or unusual symptoms. Complications are best addressed early, with the guidance of your medical professionals, to ensure a smooth recovery process.
Common Post-Surgery Complications
Adhesions, infections, and bowel obstruction are common post-surgery complications following resection of the small intestine.
- Adhesions occur when scar tissue binds nearby organs, leading to pain and potential blockages.
- Infections, though rare, can manifest as fever or inflammation at the surgical site.
- Bowel obstructions may result from scar tissue formation, causing abdominal pain and discomfort.
Promptly consulting your healthcare team upon experiencing any of these symptoms is crucial to ensure timely management and a smoother recovery process.
Preventing Complications: Tips for Patients
To prevent complications post-small intestine resection surgery, adhere closely to your healthcare team’s guidance. Thoroughly follow pre-and post-operative instructions.
- Watch out for signs of an infection, like a fever that won’t go away or pain that gets worse.
- Keep a watch on any unusual symptoms and inform your doctor promptly.
- Take good care of your wounds to lower your chance of getting an infection.
- Staying hydrated and following eating instructions will help you heal.
- Engage in light activity as advised and avoid strenuous activities until fully recovered.
Remember, your health comes first.
The Impact on Quality of Life
Living with the consequences of small intestine resection surgery can significantly impact your quality of life. Adapting to dietary changes, managing bowel movements, and possible adjustments to daily routines are common challenges.
Some patients may experience side effects such as nutrient deficiencies or bowel irregularities. Despite these challenges, many individuals find ways to lead fulfilling lives post-surgery.
Support from healthcare providers, family, and peers plays a crucial role in helping patients navigate and adjust to their new normal.
Adjusting to Life After Resection
Adjusting to life after resection involves gradually resuming normal activities while being mindful of dietary changes and potential long-term effects.
Patients may experience variations in bowel habits and energy levels. Maintaining a balanced diet rich in nutrients and regular hydration is crucial.
It is crucial to attend follow-up appointments with healthcare providers to track recovery progress and deal with any issues that may arise.
Joining support groups or community resources can also aid in adapting to the post-resection lifestyle. Consistent self-care and persistence are necessary steps on the path to optimal health.
Effects on digestion and bowel movements
After a resection of the small intestine, patients may experience changes in digestion and bowel movements. Depending on the extent of the surgery, individuals may require time to adapt to these changes.
One possible side effect that can impair nutrition absorption is short bowel syndrome. Additionally, alterations in bowel habits, such as diarrhea or constipation, may occur post-surgery.
Monitoring these effects closely and following the healthcare team’s guidance on diet and lifestyle adjustments is essential for a smooth recovery.
When to Call the Doctor
If you experience signs of infection, such as fever or increasing pain, or if you notice persistent discomfort after small intestine resection surgery, it is crucial to contact your healthcare team promptly.
Immediate medical attention is necessary for any unusual symptoms, like severe abdominal pain, excessive bleeding, or alarming changes in bowel movements.
Being vigilant about any unexpected developments post-surgery can help prevent complications and ensure a smooth recovery process.
Signs of Infection to Look Out For
Signs of infection to be vigilant about following small intestine resection surgery include persistent fever, increased pain, redness or warmth around the incision site, foul-smelling drainage, and excessive swelling.
Any signs of infection should be promptly reported to your healthcare team for evaluation and management. Early detection and treatment of infections are crucial to prevent complications and aid in a smoother recovery process.
Remember to follow post-operative care instructions diligently to minimize the risk of infections and other potential complications.
Persistent Pain or Discomfort
Persistent pain or discomfort following a resection of the small intestine should not be ignored. It could indicate complications such as bowel obstruction, incisional hernia, or infection.
If you experience ongoing pain that is severe or worsening, or if you have persistent discomfort that is not relieved by prescribed medications, contact your healthcare team immediately.
Prompt evaluation and management are essential to prevent further complications and ensure a smooth recovery process.
Conclusion
After small intestine resection surgery, follow your healthcare team’s guidance diligently for a smooth recovery. Notify your doctor immediately if you experience signs of infection, persistent pain, or abnormal discomfort.
The transition to post-operative life may require adjustments, but success stories from other patients can offer encouragement. Stay vigilant about your recovery, maintain a balanced diet with adequate fluids, and know that calling your doctor for any concerns is always the right decision.
Your quality of life post-surgery is a priority, and proper self-care plays a crucial role.
Make an Appointment
To proceed with the small intestine resection surgery, schedule a consultation with our healthcare team at +1 (817) 749-0200. Make an appointment to discuss symptoms, potential surgery options, and pre-operative assessments.
Effective management of the illness can be achieved through early diagnosis and planning. It’s essential to address any concerns or queries during this appointment to ensure a smooth surgical process.
Initiate the process promptly by contacting your healthcare provider for an appointment. Your proactive approach will contribute to a well-organized treatment journey.
Frequently Asked Questions
What Should I Expect During Recovery?
After small intestine resection surgery, expect a gradual recovery period. Initially, you may experience discomfort, fatigue, and dietary restrictions. It is crucial to carefully follow the post-operative care instructions to achieve optimal healing results. Long-term adjustments in diet and activity will be necessary for a smooth recovery process.
How Will My Diet Change Post-Surgery?
Your post-operative diet will involve a slow transition from clear liquids to solids. You should probably stay away from fatty and high-fiber foods at first. When assessing dietary intolerance, it is advisable to gradually incorporate new foods into the diet. Staying properly hydrated is essential for a speedy recovery.
Can I Lead a Normal Life After Small Intestine Resection?
Yes, after small intestine resection, many patients lead normal lives with dietary adjustments and monitoring. Following medical advice, maintaining a healthy lifestyle, and regular check-ups are crucial for a quality life post-surgery.
How to Manage Long-Term Health Post-Resection?
After small intestine resection surgery, managing long-term health is crucial. Follow a balanced diet, stay hydrated, and adhere to prescribed medications. Regular follow-ups with healthcare providers for monitoring and addressing any concerns are essential for a successful recovery.
Medically Reviewed By: Dr. Valeria Simone MD
Board-certified General Surgeon at Southlake General Surgery, Texas, USA.
Follow us on Facebook and YouTube.
References:
- Clatterbuck, Brant, and Lane Moore. “Small Bowel Resection.” StatPearls – NCBI Bookshelf, 17 Apr. 2023, www.ncbi.nlm.nih.gov/books/NBK507896.
- Mascrs, Vikram Kate Mbbs, Ms, PhD, Facs, Facg, Frcs, Fimsa, Mams,. Intestinal Anastomosis: Practice Essentials, Background, Indications. emedicine.medscape.com/article/1892319-overview#showall.
- Mrcs, Ashwin Pai Mbbs, Ms. Open Right Colectomy (Right Hemicolectomy): Background, Indications, Contraindications. emedicine.medscape.com/article/1535001-overview#showall.
- Fascrs, Juan L. Poggio Md, Ms, Facs,. Open Left Colectomy (Left Hemicolectomy): Background, Indications, Contraindications. emedicine.medscape.com/article/1965606-overview#showall.
- Mhcm, David E. Stein Md. Colon Resection: Background, Indications, Contraindications. emedicine.medscape.com/article/1891505-overview#showall.
- Small bowel resection: MedlinePlus Medical Encyclopedia. medlineplus.gov/ency/article/002943.htm.
- Small bowel resection – discharge: MedlinePlus Medical Encyclopedia. medlineplus.gov/ency/patientinstructions/000152.htm.

